Before And After: My Pancreatic Cancer

- Jaundice brings on a sudden diagnosis
- Educating myself before Whipple surgery
- Cancer in lymph nodes leads to a clinical trial
“The results of the testing clearly indicate you have a tumor on your pancreas, most likely an adenocarcinoma.”
Ask anyone who has received a cancer diagnosis and they will surely be able to tell you the day, date, and quite possibly the time the news was delivered. My Pearl Harbor Day? December 19, 2013.
Thanksgiving 2013, I started to feel a little washed out. Not a big deal, I recall. Working full-time, playing tennis three times a week, and having fun at holiday parties. Maybe a low-level flu? On December 13, 2013 (a Friday), my wife noticed my eyes looked a little yellow. My urine was darker than normal, so we made an appointment to see a doctor on Monday, December 16, 2013. After blood work (my liver function test numbers were way off the chart), an ultrasound, and a CT scan, I was admitted to Reading Hospital on December 17. The next day, after an ERCP, I was told “Your pancreas is inflamed and enlarged. Could be a tumor, but it could be pancreatitis. We inserted a stent which will allow the gallbladder to drain. Tomorrow we’ll do some further testing.”
That night and the next day I was as sick as a dog (from the bile . . . the plugged toilet flushed, so to speak). December 19, an EUS was performed to get a good close-up ultrasound picture of the area. Bile duct scrapings were collected to check for evidence of cancer cells. The initial diagnosis: Pancreatic adenocarcinoma, stage I, no suspected arterial or lymph node involvement. BOOM. My life was changed.
We were advised that I should have a Whipple surgical procedure done at the earliest possible time. A Whipple? As in Mr. Whipple? You want me to have a toilet paper salesman cut this thing out of me? Slow down, we need to learn about this thing and get educated, FAST.
Learning About the Whipple
Who should perform the Whipple (pancreaticoduodenectomy)? With the help of friends, family, and professional contacts we learned this is an abdominal procedure of extreme complexity, tantamount to open heart surgery. The history of the Whipple dates to the 1930s and Allen O. Whipple, M.D. The procedure underwent many modifications over the years, but until relatively recently consistently resulted in about a 30 percent death rate on the surgical table and a less than favorable quality of life for a significant number of those who survived surgery.
In the 1990s, John Cameron, M.D. of Johns Hopkins Hospital (Baltimore, Maryland) revised the procedure. Current mortality rates are 1 to 2 percent, commensurate with other abdominal surgeries. Most general surgeons have some experience with the Whipple, performing several or even dozens during a career. In stark contrast, I took note that Dr. Cameron had performed nearly 2,000 Whipples, followed by about 1,500 by Charles J. Yeo, M.D. (Jefferson Hospital, Philadelphia, Pennsylvania) and about 700 by John P. Hoffman, M.D. (Fox Chase Cancer Center, Philadelphia). Yeo and Hoffman both trained under Cameron. Hoffman had performed a Whipple on the mother of a close friend.
For me, the choice was clear: go with a surgeon with extensive experience. So, on December 24, I met Dr. Hoffman, who said “You have a tumor on your pancreas. Certainly not good news, but we detected it early. You’re a very lucky guy in a group of very unlucky people.” My Whipple surgery was on December 31, 2013—Happy New Year. It was a successful surgery, with clean margins. But the pathology report showed that four of 15 lymph nodes tested positive for cancer. Final diagnosis: pancreatic adenocarcinoma, stage II, T3N1.
Next Stop: Clinical Trial
The anticipated pathology of the tumor was stage I with no arterial or lymph node involvement. Had there been no arterial or lymph node involvement, my adjuvant (post-surgical) treatment would have been the then-current standard consisting of whole body radiation for one month and six months of gemcitabine (brand name: Gemzar). Since my tumor was more aggressive than was expected, Dr. Hoffman suggested we pursue alternative treatment protocols. More research.
We quickly found that even with a stage I diagnosis, the standard treatment yielded a five-year survival rate on the order of five percent, so a stage II diagnosis would have even worse odds, right? More research. Dig deeper, think outside the box. Find a clinical trial with a bigger hammer. Sounds easy, right? Wrong. The sheer volume of information related to pancreatic cancer treatments is beyond belief . . . literally hundreds of trials with every possible permutation of different chemotherapies and radiation treatments. Curiously enough, there was some, but not a lot of information available regarding immunotherapy treatments.
Since this disease is typically detected late (stage III or stage IV), the vast majority of trials we reviewed focused on treatments attempting to extend patient longevity on the order of weeks or months. Our search eventually led me to the Johns Hopkins Pancreas Multidisciplinary Cancer Clinic and a clinical trial based on the assumption that one day in the hopefully not too distant future pancreatic cancer will be able to be detected early. The trial was the first of its kind to target stage I or stage II resectable pancreatic cancer patients (me) and treat with protocols that were effective in extending longevity for late-stage patients. The regimen included six months of FOLFIRINOX, five days of SBRT (stereotactic body radiation therapy) and several doses of the Johns Hopkins proprietary GVAX immunotherapy vaccine, a cutting-edge treatment developed to supercharge the immune system of a patient to recognize and suppress the development of pancreatic cancer cells. Dr. Hoffman said, “If I were in your situation and was accepted into this trial, I would quit my job and move to Baltimore for the treatment.” I was evaluated and offered to be a trial participant, less than eight weeks after the initial diagnosis.
This was a small trial, eighteen patients in all, led by Joseph M. Herman, M.D. (a radiation oncologist now at Northwell Health in New York), Ana De Jesus-Acosta, M.D. (medical oncology) and Elizabeth Jaffee, M.D.(immunology). Interestingly, the FDA insisted patients 1, 2, and 3 in the trial were not to receive the GVAX vaccine (something about not liking having three variables in an equation, so really only fifteen candidates). As of the day I was offered the trial, patients 4, 5, and 6 had been unable to complete the chemotherapy regimen and patient 7 had succumbed to a pulmonary embolism the day after receiving the first GVAX treatment. So, there I was, patient 8 in a trial with high risk, but containing the big hammers I had been seeking. Truth be told, the next 11 months were emotionally and physically draining, but I came out the other end and was the first candidate to successfully complete the trial.
Here and Now
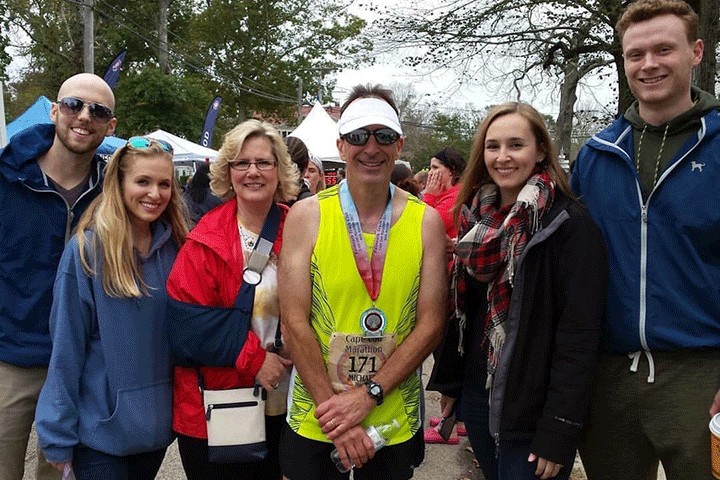
Other than a wicked scar on my abdomen and neuropathy on areas of my feet and toes, I have no other residual side effects from my treatment and have resumed normal activities. Unlike most post-Whipple patients, I have no digestive issues and do not need to take Creon with meals.
On a final note, I readily accepted the Johns Hopkins offer of semi-annual GVAX boosters, to be given “until recurrence or death,” and here I am, August 2018, almost five years post-resection, letting my breath out a bit that maybe, just maybe, I have beaten back “The Beast.”
Watch Randall tell his story on “Don’t Sweat the Small Stuff.”