What to Do If You Have Recently Been Diagnosed with Pancreatic Cancer
You or someone you love has been diagnosed with pancreatic cancer. Now what?

First, know that you are not alone in this overwhelming moment. No one should have to face pancreatic cancer without trusted resources and hope. Let’s Win is a go-to guide with content that helps patients and caregivers navigate the complexities of this daunting diagnosis. Our content is all online and designed to inform, enable, and educate with easy-to-understand, actionable information. We’ve also gathered stories from other people who have faced this difficult challenge so that you can learn from their experiences and find hope in a supportive community.
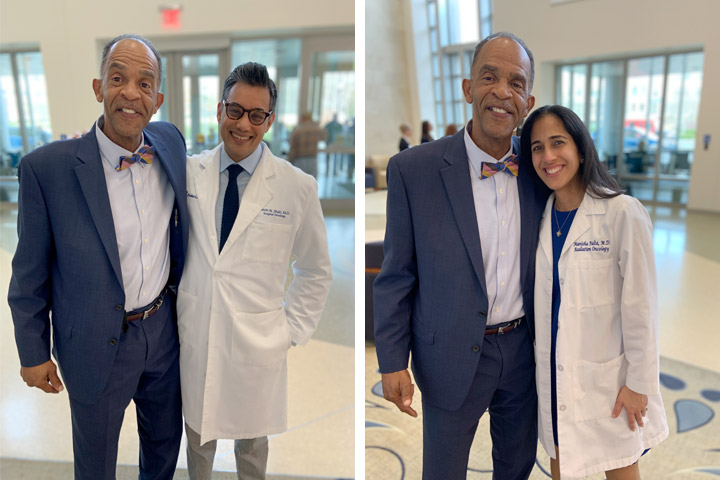
Changing Doctors Changed My Prognosis
When Camille Moses was diagnosed with pancreatic cancer, she realized she needed a doctor with an attitude that she could beat the disease.
While you may still be in shock after hearing this diagnosis, we are here to help you understand what to do. This page will walk you through the steps you may want to take as a recently diagnosed patient. We also provide links to important resources that will help you navigate the initial stages of pancreatic cancer treatment.
After Diagnosis
Knowledge is power. So do your research. You want to know exactly what you are dealing with so that you can make informed decisions as you start treatment. Use every opportunity to ask questions, so you can better understand the path forward.
Gather Information
- Complete all necessary tests, which may include scans, scopes, and bloodwork.
- Learn the tumor location, type, and stage. Understanding these aspects of your disease will impact your treatment plan. For more information on pancreatic cancer staging, visit our Stages page.
- Obtain genetic testing through blood or saliva samples. All newly diagnosed pancreatic cancer patients should have genetic testing to determine if they have certain inherited genetic mutations, regardless of family history. This information may guide your treatment plan and can be helpful to family members. Genetic testing is now considered part of the standard care for pancreatic cancer and a genetic counselor can help you make sure it is covered as part of your treatment. Our genetic testing pages have more information about how to get tested.
- Obtain molecular profiling of your tumor if possible. This test can identify whether your tumor has mutations in specific genes that may make it respond better to certain treatments.
- If you can, bring a friend or family member with you to your appointments. Two people listening, absorbing, taking notes, and asking questions are better than one, especially when so much information is being shared. It’s especially helpful to create a list of all questions prior to your doctor appointment. Remember that there are no dumb questions!
Get a second opinion
- It is helpful to get a second opinion from a medical center that has a pancreatic cancer program, where the oncologists will know about the latest treatments. Our Doctor Finder highlights specialists. In addition, many major academic medical centers have formed partnerships with regional hospitals, so an experienced specialist may not be that far away. And most insurance plans, including Medicare, cover second opinions for major illnesses. The National Pancreas Foundation has an up-to-date list of Pancreatic Cancer Centers of Excellence, which may also be helpful.
Choose your treatment team
- Find oncologists who are experienced in treating this cancer; they are more likely to know about the latest treatments. We have downloadable lists of major teaching hospitals and cancer centers in the U.S. and Canada to help you with your search for treatment.
- If you are able to have surgery to remove the tumor, find a surgeon who has performed many pancreas surgeries. Surgery for pancreatic cancer is complex, and you are much more likely to get better results with an experienced surgeon.
- Your treatment may involve a combination of therapies, including chemotherapy, radiation, and surgery, requiring an interdisciplinary team.
- If your cancer treatment center includes a nurse navigator, he or she can help you coordinate treatment and visits.
- Continue to see your primary care physician and specialists for other conditions that you may have. Encouraging and facilitating open communication between everyone on your care team is key. Don’t be shy.
Consider clinical trials
- Clinical trials offer the latest options for the treatment of pancreatic cancer, and while some participants may receive the new drug or treatment being tested, ALL participants receive the standard treatments. Visit our Trial Finder for more help.
Contact your health insurance company
- Educate yourself about your health insurance coverage and any deductible you may have. Learn which physicians and facilities are included in your plan, and which ones are out of network.
- Seek advice on how you will handle the financial responsibilities of treatment.
Resources
- Visit the websites of pancreatic cancer organizations such as Let’s Win, the Lustgarten Foundation, Pancreatic Cancer Action Network (PanCAN), and others, to learn all you can about pancreatic cancer, its treatments, clinical trials, and other resources to help you at this critical time.