Surviving Pancreatic Cancer and Inspiring Others
- Pain and jaundice lead to pancreatic cancer diagnosis
- Recovering from pancreatitis before traveling to a specialist
- A Whipple procedure followed by chemo
- Radiation and more chemo
Sometime in 2008 I started having a dull pain on my right side.
I was 53 years old, exercised regularly, and had a healthy lifestyle. My PCP suggested the pain was being caused by my gall bladder and told me to lay off fatty and greasy foods. I did and the pain subsided. Between 2008 and July 2010 I kept to a fat-free diet and added more exercise. The pains would come and go, so my PCP ordered sonograms and a did a scan of the gall bladder—both were negative.
In July 2010 I was coming home to Chesapeake, Virginia, from a business trip, when I began having severe pains on my right side. I also noted I was turning yellow, suggesting jaundice. When I got home, I went to the local outpatient clinic. When I gave a urine sample, I saw it was the color of coffee. By this time, I had turned a deep yellow and could not stand due to the pain. The doctor at the clinic told my wife to take me directly to the hospital ER—they would call ahead and notify the hospital I was coming and needed to be seen right away.
At the hospital I was admitted right away and Dr. Pramod Malik, a GI doctor (now at Sentara Healthcare in Suffolk, Virginia), was called in. He did an endoscope exam and noticed a growth around the common bile duct. He also noted the jaundice and inserted a stent in the bile duct to free up the bile that was backing up in my system. After the stent was inserted, I had painful cramps in my abdomen, which turned out to be pancreatitis. This was thought to be caused during the procedure of inserting the stent when my pancreas was bumped, causing it to become inflamed. The hospital I was at had very little experience with this situation and at the time there were no specialists in my area to give assistance.
Next Stop Baltimore and Pancreas Experts
The GI doctor did some research and found that Johns Hopkins Hospital in Baltimore, Maryland, was the largest hospital dealing with issues of the pancreas. The GI doctor made arrangements for me to get an appointment at Hopkins but due to the pancreatitis I was unable to travel the five hours from Chesapeake to Baltimore. I remained at our local hospital while the doctors worked to get the pancreas to calm down. I could not eat any solid food, so a peripherally inserted central catheter (PICC) line was inserted and I was given total parenteral nutrition (TPN) to bypass my digestive system.
I stayed at the local hospital from July 19 to 25 and then went home, although I remained on the PICC line. By mid-August I was well enough to go to Hopkins. At Hopkins I was diagnosed with pancreatic cancer. The pancreas was still inflamed, so no solid food and the PICC line stayed in. I went a total of 38 days without any food—only TPN. I lost over 40 pounds and much of my strength. Finally, at the end of August, the PICC line was removed and I could start a diet of solid food. The first meal I had was at Hopkins—roast beef with mashed potatoes, mixed vegetables, and gravy; I can still taste it.
From September through October I had to go back to Hopkins every two weeks for checkups and CT scans to monitor the tumor. In 2010 no other tests were used to determine the type of tumor and there were minimal treatment options.
Treatment Finally Begins with a Whipple
The surgery for the Whipple was scheduled on November 3, 2010, with Dr. Frederic Eckhauser (now retired and in Wilmington, North Carolina) at Johns Hopkins Hospital. The operation lasted 10 hours and I was in the hospital for 12 days. My wife stayed in the hospital the entire time with me—she was a great comfort and relief. By mid-November we were able to travel home, where I continued to heal and recover.
On January 4, 2011, I started chemo treatments here in Chesapeake. The only drug available was gemcitabine. The treatment regimen was three weeks of chemo one day a week and then one week off. This continued for three months. After this I was off for one month to recover and then started 25 treatments of radiation with chemo. The radiation was performed at Johns Hopkins and the chemo drug was Xeloda. Radiation was five days once a day and then weekends off. I had to stay at a hotel during treatment. I was also working full-time from the hotel. I would get treatment in the morning and see clients during the day. By the third week of radiation I was extremely weak, so my wife came up to help me. She would take me to radiation and then drive me to my appointments. We did this for the last three weeks of treatment.
In June I went back home and started the next round of chemo with gemcitabine and the same regimen—three weeks on and one week off for three months. Also, during this time, we had to travel back to Hopkins for CT scans every two weeks. Each scan was promising, with no signs of the tumor or any other cancers forming.
I continued getting CT scans at Hopkins every three months all through 2012 and 2013. Then the scans were every six months from 2013 through 2014. By 2015 I graduated to once a year and in October 2017 I had fully graduated—no more CT scans!
Finding an Organization that Helps
All during our journey my wife and I were in the dark and did not know about any organizations that could support or help us. We did not hear about clinical trials or other experimental therapy options. All we knew was that the survival rate was 6 percent.
During my checkup at Hopkins in 2012 I was coming to grips that I was not only a cancer patient but also a survivor. I had the desire to help others but did not know where to turn or how to begin. I asked my medical oncologist Dr. Joe Herman (now at Northwell Health in New York) what was a “good” organization to volunteer with and help others with pancreatic cancer. That’s when I first heard about PanCAN. Dr. Herman was on their medical board and he said they were an outstanding, well-run organization. We had not heard of PanCAN or anything else on pancreatic cancer but when I got home, I looked them up on the web and found a listing of their affiliates. I saw they had one in my area, then called the “Tidewater Affiliate” (now the Virginia Beach Affiliate).
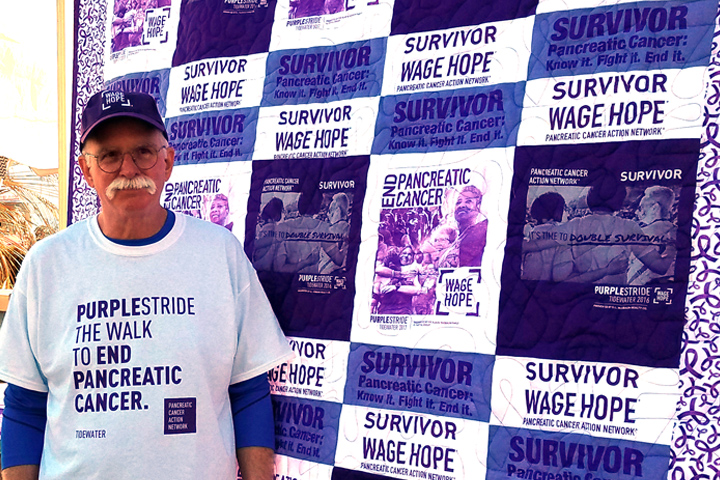
Since I started to volunteer with PanCAN the experience has taken me out of my comfort zone. I have spoken at various events such as PurpleLight and on local TV shows for PurpleStride. I have appeared in two news segments on Channel 10, a local news station, and my story has been written up in local newspaper articles. I have also had the honor to meet so many survivors; some have since passed on, but they all contributed to the body of knowledge that has helped to improve treatment options.
I am now listed on the PanCAN website for Survivor & Caregiver Network. I receive calls from patients across the U.S. I have also started to make quilts for patients going through treatment. I also make quilts to sell at various events such as craft shows to help raise money for PanCAN. The quilts have been a major ice breaker in getting information into the public arena. I have displayed quilts at various shows and events in Hampton Roads and Elizabeth City, North Carolina. A number of local newspapers have written features on me and my quilts.
Since my diagnosis I have had the pleasure to witness the survival rate increase from 6 percent to 10 percent, clinical trials are now a valid option, and there are more chemo treatments to help shrink and contain the tumors, making surgery more successful. But we still have a long way to go.
Watch John tell his story in “A Bright New Future.”






