Vigilance Leads to Pancreatic Cancer Diagnosis

- Mild symptoms lead to scan, which leads to diagnosis
- Strong chemotherapy
- Surgery to remove the tumor
- Post-surgical chemotherapy
My story begins November 3, 2010.
While my wife and I were on vacation in South Carolina to celebrate my 70th birthday, I started having night sweats. I am an ophthalmologist, and on returning home I went to my internist. He found an elevated white blood cell count, indicating active infection. We investigated the usual culprits—urinary tract infection, kidney infection, among others—and found nothing. I began to suspect tuberculosis (TB), because as an intern many years ago I performed mouth-to-mouth resuscitation on a patient who was later found to have a highly infectious form of TB. I was treated at the time but never developed active infection. I knew it could show up many years later, but again nothing was found.
One day in my office I was with a patient who was very upset about her sister who had just died from pancreatic cancer. Her symptoms were not typical—no pain or GI discomfort, just some tiredness and a low-grade fever. I called my internist and asked him to order a CT scan of my pancreas. He laughed and said no way, but he ordered it.
On the evening of November 3 my oldest daughter, an internist, came running into the house in tears. She had gotten my CT results right away. A 6-centimeter tumor was found on the distal pancreas with two possible metastatic lesions in the liver. Talk about one’s life changing.
Confirming the Diagnosis
We immediately saw a surgeon, who called a GI specialist to do a pancreatic biopsy. Prior to the procedure he assured me that it was probably a cyst. He said that he does these all the time and l looked too good to have cancer. He said he would call in early evening with good results. By 10 p.m. we still had no call, so my daughter called him and got through. “He’s got the worst variant of adenocarcinoma,” the GI specialist told her.
The surgeon said he would take me to the operating room, use a scope to get a better look, and if all looked okay he would operate. I awoke in recovery, with no tubes and just a small incision. The surgeon had met with my family to inform them I had inoperable cancer and advised them to let me go. “He’ll die relatively comfortable in three months; chemo might give him six but it will be pure misery.”
Finding Treatment
We went to Memorial Sloan Kettering (New York) and received the same news. My daughter knew an oncologist (now retired) in Albany, New York, that people were raving about. He said, “Let’s try chemo.” So I started on a three-day regime of oxaliplatin, irinotecan, and leucovorin intravenously, then at home I was hooked up to a continuous drip of fluorouracil for two more days.
After two weeks of this I was hospitalized in isolation with a life-threatening low white blood cell count. I couldn’t even shave with a razor. The slightest nick, if infected, could kill me. We decided to do the treatment every two weeks.
After four months of this poison I had lost 30 pounds and endured many side effects—terrible weakness, sores in every orifice of my body, among others. My wife and I watched cooking shows to help my appetite. What l ate was all anti-cancer stuff—I’ll never look at kale again.
One day while waiting to see my oncologist I caught his eye down the hall. He turned, looked at me, and gave me a thumbs up. WOW—the tumor had shrunk to 2 cm! “Maybe, just maybe, you’re operable,” he said. “Let me call a friend at Sloan who is a little more aggressive.” Off I went to see Dr. Yuman Fong (now practicing in California). Dr. Fong asked me, “Are you a glass half full or glass half empty person?” As an eternal optimist l decided to go ahead with the surgery.
In recovery I awoke again with no drains. They closed me up, but then looking down my gown I thought, “That’s the largest laparoscopic incision I’ve ever seen.” The drapes parted with Dr. Fong and my family all smiling. “I think we got it all,” he said. I went home after a week and was on three months of gemcitabine (a much milder form of chemo).
Life Post Treatment
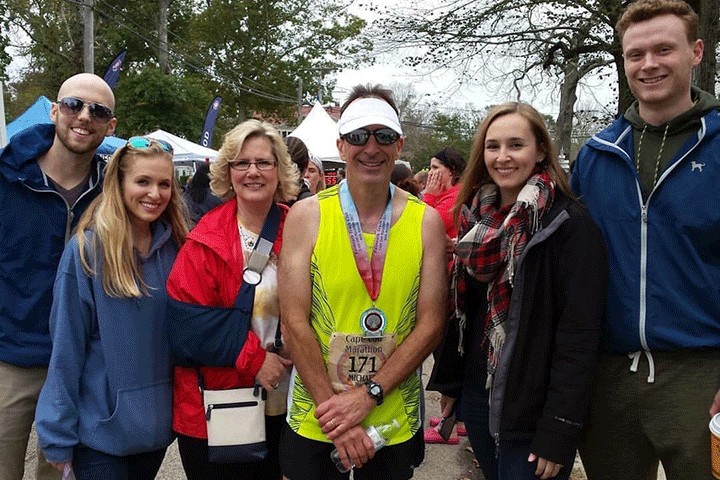
I had regular scans for years, but in 2017 l said to my oncologist, “You’re gonna kill me with radiation rather than cancer. Let’s stop the scans.” He agreed. “We’ll just do the tumor marker blood test every six months.” With my magnificent family, wonderful friends, and a great deal of prayer (I took care of most of the nuns in Albany), I am doing well. We just celebrated our 58th anniversary and I feel great. How fortunate am l.
Watch Michael tell his story in “Listen to the Patient.”