Aiming to be More than a Statistic

- Jaundice leads to pancreatic cancer diagnosis
- A Whipple procedure followed by chemotherapy
- Rising tumor marker and a change in chemotherapy
- After a search, finding a clinical trial
I am a Board Certified general and plastic surgeon. On July 31, 2014, I was in surgery, finishing a case, when my nurse looked at me and said, “Do you know your eyes are yellow?”
I felt fine, with no immediate medical problems, so I was surprised to hear her say this to me. After finishing the case, I went to the dressing room, looked in the mirror, and confirmed the jaundice of my eyes. I went straight to the lab, and had a complete medical profile done on a blood sample. As a surgeon I know that the most common cause of painless jaundice is pancreatic cancer, until proven otherwise.
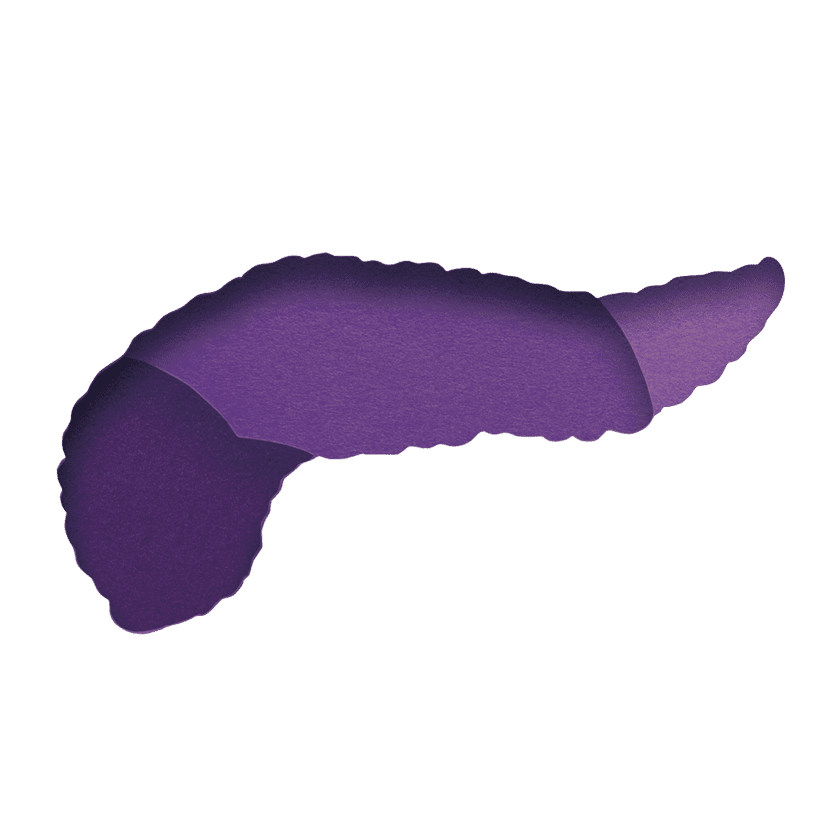
I picked up my blood results the next morning. My hematology was normal, but my liver function tests were wildly elevated. This confirmed my fears. A CT scan the next day showed an obvious 2.5 cm mass at the head of the pancreas, which most likely was an adenocarcinoma.
Starting with Surgery
I discussed these results with my wife, and we decided to have the surgery performed, if possible, in my home hospital in Oklahoma City, because our transplant center has excellent surgeons. I chose Dr. John Duffy at INTEGRIS Baptist Medical Center, called him immediately, and went over my test results with him. He agreed with my diagnosis and further added that the tumor did not appear to involve the superior mesenteric vessels, indicating that I would be a good candidate for the surgery, despite my age (76).
On Friday, August 8, 2014, I underwent an eight and a half-hour Whipple procedure, which removed my gallbladder, anterior third of my pancreas, one-third of my stomach, and my duodenum. This major rearrangement of my intestinal plumbing was a big endeavor, with equally strange results to my diet, weight control, etc. Pain was another major problem, as was protecting the eight drains and tubes exiting my abdomen through the skin. To keep me going during my residence in the ICU, I had six IV lines connected to bags of various liquids (one of which was for pain control).
After the surgery, my pathology report said I fortunately had clean margins, and the entire tumor was removed, but two lymph nodes were positive for tumor cells. I was classified as a T2N2M0, which means that the tumor was larger than 2.5 cm, two metastatic lymph nodes were found, and there were no distant metastases.
My Treatment Protocol
Eight days post Whipple, I went home to finish healing. All drains out!
I saw Dr. Brian Geister at the INTEGRIS Cancer Institute to plan my chemotherapy. A month later I had a port inserted and started a regimen of gemcitabine and Abraxane every three weeks for six months. During this time, my CA 19-9 tumor marker and CT scans, every three months, were normal. When I took a “chemo holiday” for two months, my CA 19-9 started to rise, so I started another six-month course of the same drugs. I stayed on these drugs until the end of 2017. When necessary I got shots of Neulasta for my falling white cell count, and Procrit for my anemia. I was fortunate to have minimal side effects, mainly fatigue and occasional diarrhea. Luckily, I did not become diabetic as a result of the surgery.
Because I tolerated the chemo well, I went back to work as a plastic surgeon two months post Whipple. The work kept me occupied and helped fight off depression, knowing the statistics for pancreatic cancer. My quality of life was almost normal, except for fatigue. I worked, traveled, gave lectures, socialized with my wife, water skied, and went scuba diving.
The Importance of Genomic and Serum Testing
As a surgeon who has now read volumes about pancreatic cancer, I believe genomic testing and immune therapy is the treatment protocol of the future, getting away from the cell-poisoning drugs used today for chemotherapy. Because of my research, I sought out suggestions for clinical trials from Pancreatic Cancer Action Network (PanCAN). I traveled to both Dana-Farber (in Boston, my hometown) and MD Anderson (in Houston) for consultations. Both research centers turned me down because I had no visible metastases on PET, CT, or MRI scans. While I considered not having mets a blessing, it kept me from the trials.
While I was undergoing chemo I decided to have my genome studied. I found out that I have four mutations. I am BRCA normal, but have an ATM and KRAS mutation, as well as two other minor mutations.
My bubble broke in November 2017, when my CA 19-9 started to rise higher than after surgery, and did not respond to the usual regimen of gemcitabine and Abraxane. PET and CT scans revealed two positive lymph nodes in the surgical bed of the pancreas resection.
I wanted a serum biopsy but was told this test is not approved for pancreatic cancer. On the advice of Dr. Laura Miles, a local physician with whom I consulted, I sent 15 cc of my blood in a special container and $5,000 to a lab in Greece. The lab determined I had seven malignant cells per ml of blood—a high number. The lab then tested the cultured cells against all existing chemotherapeutic agents. This helped determine my chemo regimen and subsequent switch to FOLFOX in December 2017. It upset me that I could not get this test done in the U.S. The FOLFOX began to work, and slowly my tumor marker decreased, but not to normal.
On a Clinical Trial
Through PanCAN I found out about the research being done at the University of Pennsylvania (Abramson Center). My daughter is a professor of critical care veterinary medicine at Penn, and I am a graduate of the medical school. We contacted Dr. Robert Vonderheide, whose staff was most gracious, and he invited me to come for a consult. We scheduled my first visit in April 2018, and I met Dr. Kim Reiss Binder, who actually seemed excited to meet me and described a new study testing a PARP inhibitor plus a checkpoint blockade agent designed for patient survivors who had been on FOLFOX and had metastatic disease. She and her staff were truly like family, and I felt very comfortable in their care, and enrolled in the study.
I have stopped FOLFOX, and now must travel to Philadelphia every two weeks for the infusion and pills. Fortunately, my port is still open almost four years since its insertion. As of June 29, 2018, I have had three treatments, with the fourth scheduled next week. I have had minimal side effects except for peripheral neuropathy in my fingers and fatigue. Actually, I feel better now than I have since my surgery.
I will be 80 years old on July 11, 2018, and am four years post-diagnosis and Whipple procedure. My wife (an ophthalmologist) and I remain in Oklahoma City, OK. I retired from my practice of plastic surgery last year and have assumed the role of “house husband” and gardener. I still consult on medical cases when asked, and have maintained my CMEs and medical license.
I fully believe that, with the help of God, Dr. Duffy, Dr. Geister, and my wife saved my life so that I can become a pancreatic cancer statistical outlier. Whether my new experimental protocol will suppress my tumor and keep me off FOLFOX, only time will tell. Speaking of time, I am grateful for every day I wake up in the morning and feel reasonably well. My wife makes sure I eat a healthy diet and maintain my weight. I take several nutritional supplements thought to increase the strength of the immune system. Good diet, exercise, positive attitude, and a good support group are essential to beating or suppressing this very fatal disease.
Paul passed away almost seven years after his pancreatic cancer diagnosis. He used his understanding and expertise as a physician to seek out a clinical trial, which helped him and extended the knowledge for other patients. We offer our deepest sympathy to his family.