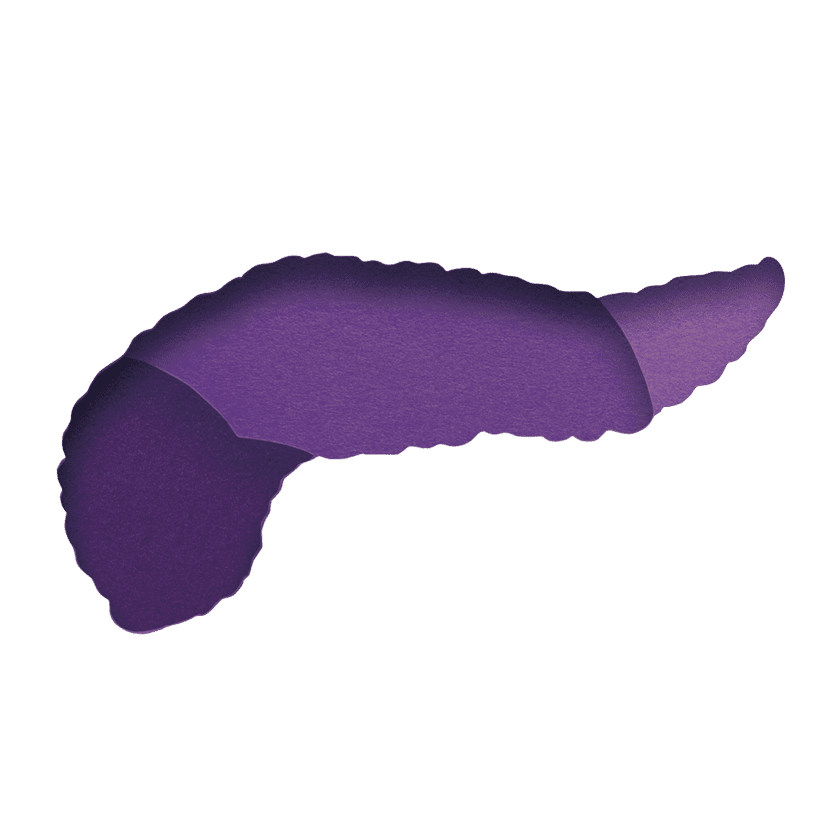
Five Promising Researchers Leading the Charge in Treatment Advancements

Whether it’s exploring the cargo of extracellular vesicles or harnessing artificial intelligence to deliver better patient care, early career scientists are often on the cutting edge of innovation.
Which is why we were once again happy to support the attendance of five pancreatic cancer investigators to the 2023 AACR Special Conference in Cancer Research: Pancreatic Cancer. Learn more about these inspiring individuals and the research they presented.
Joel Encarnación-Rosado
Targeting pancreatic cancer metabolic dependencies through glutamine antagonism
From quantum dots to cell metabolism and “self-cannibalism,” Joel Encarnación-Rosado has had a well-rounded early research career. As a Ph.D. candidate and HHMI Gilliam Fellow at the New York University Grossman School of Medicine (New York City), Joel has been working in the lab of Alec Kimmelman to dive deep into pancreatic cancer metabolism. The research presented at AACR involves targeting pancreatic cancer metabolic dependencies through glutamine antagonism.
“Glutamine is an important metabolite for cancer and normal cells. Previous attempts to target glutamine metabolism in cancer patients resulted in high toxicity. Our work investigates the role of a recently developed drug that targets the utilization of glutamine only in cancer cells, avoiding the toxicity issues.”
Beyond the bench, Encarnación-Rosado is also an advocate for more diverse voices and culturally relevant role models in the biomedical workforce. Encarnación-Rosado obtained his B.S. at the University of Puerto Rico, Rio Piedras Campus, where he was an NIH-funded RISE and MARC fellow.
Jennifer Finan
Unraveling the importance of pancreatic cancer extracellular signaling to endothelial cells within the tumor microenvironment
Trained as a biochemist at St. Lawrence University in Upstate New York before working as a research technician in a cancer metabolism lab at the University of Pennsylvania, Ph.D. candidate Jennifer Finan now has her sights set on unraveling the importance of extracellular vesicle crosstalk in pancreatic cancer.
Extracellular vesicles are released from cells and can carry a variety of biomolecules, including proteins, lipids, and nucleic acids. “These small particles used to be thought of as cellular trash, but we are now understanding that they are cell signaling messengers, containing contents that are highly regulated and that can impact surrounding cells both nearby and far away by traveling through the blood or lymphatics,” Finan explains.
Working in the lab of Dr. Jonathan Brody at Oregon Health and Science University (Portland), Finan is investigating which cells within pancreatic tumors are importing these cancer extracellular vesicles, and how this impacts the surrounding normal cells. The lab has also shown that an RNA-binding protein, HuR, can regulate genes important for tumor cell survival, and Finan is assessing how this protein impacts the cargoes and functions of pancreatic cancer extracellular vesicles.
Kristen John
Implementation of a real-time AI-guided navigation service for pancreas cancer
Kristen John is a third-year medical student at the Donald and Barbara Zucker School of Medicine at Hofstra/Northwell (Hempstead, New York), where she works under the mentorship of GI oncologist Daniel King, M.D., Ph.D. She previously worked at Cold Spring Harbor Laboratory, where she used CRISPR/Cas9 to identify the correct molecular target of previously mischaracterized anticancer drugs, and at Dana Farber Cancer Institute, where she led an independent project to characterize the pancreatic ductal adenocarcinoma (PDAC) immunopeptidome after irradiation and immunotherapy treatments.
At the AACR Pancreatic Cancer conference, John presented the results of the pilot implementation of an AI-guided identification and navigation service for patients with pancreatic cancer.
“In the first month of implementation alone, we found that we were able to improve care delivery in several ways, including identifying patients earlier in the diagnostic timeline; decreasing time from date of radiology report to biopsy (from 22 to 7 days), outpatient visit (from 32 to 15 days), and treatment initiation (from 56 to 34 days); and nearly tripling our monthly biospecimen accrual rates.“
John also has an interest in health equity and cancer disparities, presenting a study regarding the rates of unplanned hospital care in Black Americans with pancreatic cancer at the 2023 ASCO Gastrointestinal Cancers Symposium. The study motivated a quality-improvement pilot project in which computational identification is used to prospectively find these patients and provide culturally tailored outreach via phone call from an African-American nurse practitioner who evaluates their healthcare vulnerabilities, social determinants of health, and factors leading to their emergency department visits in real time.
Zeribe Nwosu
Uridine-to-ribose axis supports glucose-restricted pancreatic cancer
What are the molecular mechanisms and microenvironmental features that alter cancer metabolism, contribute to cancer aggressiveness, and lead to resistance to treatment? Are there new gene signatures or biomarkers that could lead to earlier diagnosis or better treatment of cancer? Dr. Zeribe Nwosu has devoted his career to finding out.
At AACR, Nwosu presented his research into pancreatic cancer metabolism and potential ways to achieve treatment by starving the tumors of their preferred nutrients, in this case glucose and uridine. Right after this conference, he transitioned to a new position as an NIH Cornell Faculty Institutional Recruitment for Sustainable Transformation (FIRST) Assistant Professor in the Department of Molecular Biology and Genetics at Cornell University (Ithaca, New York). His plan is to continue to identify and characterize nutrient transporters, novel enzymes, oncogenic signaling, and transcriptional or epigenetic regulators or cellular components in the tumor microenvironment (e.g., immune cells, fibroblasts) that enable cancer cells to “feed” and grow.
Prior to joining Cornell, Nwosu obtained his Ph.D in Molecular and Cellular Biology from the University of Heidelberg, Germany, and did his postdoctoral research in the labs of Dr. Costas Lyssiotis and Prof. Marina Pasca di Magliano at the University of Michigan.
Born and raised in Nigeria. Nwosu also established the Zeribe Nwosu Foundation (ZNF) to advance the education of Africans at all levels, through seminars and learning activities, mentorship, and scholarship.
Lucy Oldfield
Deep proteomics identifies novel biomarker candidates and molecular pathways of pancreatic cancer-related diabetes
Dr. Lucy Oldfield is a senior postdoctoral researcher in the department of Molecular and Clinical Cancer Medicine at the University of Liverpool (United Kingdom). She holds a Ph.D. in Analytical Chemistry from the University of West Virginia, an M.Sc. in Forensic and Analytical Chemistry from the University of Strathclyde and an M.Sc. in Chemistry from the University of Manchester. Her work for the past several years has focused on biomarker development for early detection of pancreatic cancer, especially using proteomics techniques. Oldfield is interested in the relationship between pancreatic cancer and diabetes, including the mechanisms underpinning the development of diabetes in individuals with pancreatic cancer.
At AACR, she spoke about her project to identify protein biomarkers that distinguish type 3c diabetes (which includes pancreatic cancer-associated diabetes) from type 2 diabetes, paving the way for the development of diagnostic tools capable of selecting individuals for pancreatic cancer screening at the point of diagnosis of diabetes. As part of this research, her team has undertaken the deepest interrogation of the human plasma proteome for biomarkers of pancreatic cancer to date. Using state-of-the-art technologies, including an aptamer-based platform and mass spectrometry, they have measured ~7,500 proteins in individual plasma samples from disease groups selected to address early diagnosis of pancreatic cancer in individuals with new-onset diabetes. A small panel of promising proteins has been isolated and validation is planned. Oldfield’s team will also use their data to investigate the molecular mechanisms at play in pancreatic cancer-related diabetes, to help better understand the biology underpinning the onset of diabetes prior to pancreatic cancer diagnosis.