New Potential Early Detection Trial for Type 2 Diabetics

Although uncommon overall, pancreatic cancer is a deadly disease—ranking as the third most frequent cause of cancer death in the United States.
Unfortunately, most cases of pancreatic cancer aren’t found early enough to be treated with surgery, which is considered the only potential cure for the disease.
Pancreatic cancer screening of asymptomatic adults is not generally recommended because of the relative rarity of the disease, the lack of an effective screening test, and the potential to do more harm than good with unnecessary scans and tests. Researchers are studying and recommending surveillance programs for individuals who are at higher risk of the disease. This includes people with familial breast, ovarian, or colon cancer or an inherited genetic syndrome associated with pancreatic cancer; pancreatic cysts; or chronic or hereditary pancreatitis.
But pancreatic cancer is a tricky beast. Smoking, age, obesity, and diets high in red and processed meats also play a role in risk, and Black Americans are diagnosed at a higher rate than other Americans. Type 2 diabetes is also being studied for its role in risk of pancreatic cancer.
A 2005 population-based study published in the journal Gastroenterology looked at more than 2,000 patients who were at least 50 years old with newly diagnosed type 2 diabetes for the development of pancreatic cancer within three years of initial diagnosis.
Of the 2,122 patients with diabetes, 18 were diagnosed with pancreatic cancer within three years. This represented a three-year incidence of nearly eight times that of the general population. The study concluded that 1 percent of people with diabetes aged 50 or more will be diagnosed with pancreatic cancer within three years of first meeting criteria for diabetes.
In the nearly two decades since that study was first published, ongoing research is starting to better clarify that risk and how diabetes and pancreatic cancer may be linked. A clinical trial called New Onset Diabetes Management for Earlier Detection of Pancreatic Cancer, dubbed NODMED, is now underway. The study is focusing on patients with new-onset type 2 diabetes. Its purpose is to evaluate the performance of a newly developed blood-based early detection pancreatic cancer test in a clinical setting. The test was developed by Bluestar Genomics, now called ClearNote Health, of San Diego, California.
Detecting Cancer Early
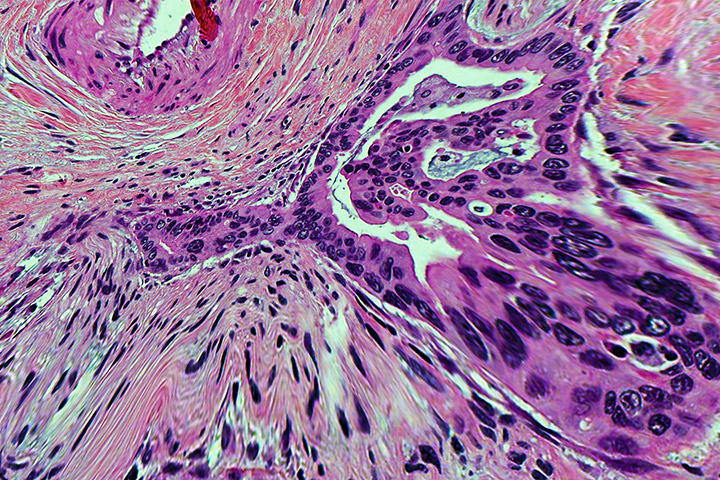
These cancer-seeking blood tests are often referred to as liquid biopsies. For example, a study of one blood test aiming to identify more than 50 different cancers looks at a kind of molecular signature or pattern embedded in the cancer DNA that identifies the tissue it came from. These signatures are a result of DNA methylation, a naturally existing modification to the surface of DNA. Cancer cells have abnormal DNA methylation patterns, and these patterns correlate to the type of cancer invading the body. Using high-tech methods, scientists can create a kind of index of these DNA methylation patterns. Multi-cancer detection tests might be able to home in on the sections of DNA that distinguish between cancerous and normal tissue as well as pinpoint the site of origin.
Others, like ClearNote’s pancreatic cancer test, which is called Avantect, focuses specifically on just one cancer. “We are really zeroing in on a tailored, precise approach,” explains molecular oncologist and vice president of product development Anna Bergamaschi, Ph.D. That approach, she says, differs from the “broader catch-it-all” tests, thus improving both sensitivity and specificity for pancreatic cancer.
The engineering behind the Avantect test relies on a combination of both genomic and epigenomic information. Epigenetics refers to how your behaviors and environment can cause changes that affect the way your genes work. Epigenetic changes don’t change your DNA sequence, but they can change how your body reads a DNA sequence. Epigenetic changes include DNA methylation as well as a process called demethylation. Typically, methylation turns genes “off” and demethylation turns genes “on.”
Avantect is designed to measure a biomarker with the impossibly long name of 5-hydroxymethylcytosine, referred to as 5hmC. This biomarker is actually a product in the active demethylation of 5-methylcytosine, or 5mC, a methylated form of the DNA base cytosine.
The test essentially tracks gene activity and cell changes. “What happens is that the technology tags those DNA fragments that contain 5hmC so they can be sequenced,” Bergamaschi explains. Once the 5hmC profiles in a patient’s blood are profiled, a biomarker set is developed through machine learning algorithms. “We are looking at active biology,” adds Bergamaschi. “So the information we get from 5hmC, along with the sequencing of the whole genome through machine learning, gives a signature of cancer. All with just one simple blood test.”
A large case-control study included 2,150 patients, 2,048 without cancer and 102 with pancreatic cancer. Those patients, all over age 50, included individuals with a family history/genetic predisposition to pancreatic cancer, as well as those with newly diagnosed type 2 diabetes or longstanding type 2 diabetes, heavy smokers, and those of average risk. The test was found to have a sensitivity for early stage pancreatic cancer of 68 percent and a specificity of 97 percent.
An extension of the same case-control study compared the effectiveness of the assay to the biomarker CA 19-9, which is regularly used for understanding how pancreatic cancer responds to treatment. But the CA 19-9 test isn’t always reliable because some people with pancreatic cancer don’t have elevated CA 19-9 levels. Results showed sensitivity of the ClearNote test to be 75.8 percent compared to CA 19-9 at 57.6 percent in early stage cancers.
More about NODMED
This is a multisite study of the ClearNote test that will follow participants over a long period of time, gathering information and observing outcomes and the direct impact of the test. Researchers hope to enroll 6,550 men and women, 50 years of age and older, diagnosed with type 2 diabetes within 90 days prior to enrollment.
The study will include two cohorts: those 50 to 64 years of age and those 65 and older. MRI imaging (or alternate imaging if subject is unable to undergo MRI) will be performed on subjects whose test result is “detected.”
If the imaging study results are abnormal, the subject will be referred back to their enrolling clinician for additional diagnostic work as part of routine healthcare. If pancreatic cancer or any other pancreatic lesion is diagnosed, the diagnostic reports will be collected as part of the study’s clinical data.
“Pancreatic cancer is a terrible disease, and too many people are diagnosed at later stages of the disease. So potentially giving people more time, more precious moments, through early detection is very important,” Bergamaschi says.
“Getting to the point of developing a test, making it fully automated, doing a validation study, and getting it into a clinical trial is rewarding. There have been a lot of challenges, don’t get me wrong. I’ve had a tough day, but never a bad day.
“I am very excited about this, so excited that I texted my colleagues at 4 a.m. when I found out another patient enrolled [in the trial]. My colleagues said I should be sleeping. But as a scientist, this is a passion.”