What Is It Going to Take to Stop Pancreatic Cancer? A 10-Year Survivor’s Perspective

When my daughters were still in elementary school, we would pile everyone into our 2002 Nissan Quest minivan and set off on a road trip.
After the girls were bounced around for a few hours, their murmurs from the back began to swell. First, it was, “I’m bored.” Then, “My sister is in my space.” Followed by “Don’t touch me!” Then came the words no parent ever wants to hear: “When will we get there?” Being a 10-year survivor who was certain he was done, I have to ask the same thing, “When will we get there?” What is it going to take to stop pancreatic cancer?
While I’m beyond thankful to still be here 10 years later, as well as for the hard work of organizations like Let’s Win along with the Lustgarten Foundation and the Pancreatic Cancer Action Network (PanCAN), we need to do more, much more.
Unfortunately, a resource like Let’s Win did not exist back in 2013 when all this began for me. I had questions about my questions. Everything I read said it was over for me. I didn’t know where to turn. Hope was a four-letter word to me. I had none. I still remember being swamped by sadness thinking I would not be there for any of my three daughters’ big days. Thankfully, two of them are now married. I’m holding out for the third, my baby.
Toll of Pancreatic Cancer Not Acceptable
With more than 50,000 people dying from this hideous malady each and every year, almost the equivalent of American soldiers killed in Vietnam over 10 years, more funding needs to be made available to unravel this knotted mystery. Would we accept a Vietnam, with its death and destruction, every year? I think not. So why are we?
Of course, everyone believes “their cancer” is special. But with only 12 percent of those getting told “I’m sorry, you have pancreatic cancer” seeing five years, a strong case can be made for increasing the funding for research for this cancer. Yes, it is special.
Need for Additional Funding
As a first step, this additional funding should be focused on developing an early detection test to find it before it’s too late. A big reason why most don’t survive is that it often has no symptoms and is found too late to do anything to stop it. A few might experience indigestion or twisting stomach pain, but most are oblivious until a scan reveals a mass in or around the pancreas. Patients today are screened for pancreatic cancer with a CA 19-9 tumor marker protein test. But one thing is clear: This protein test standard is wholly unreliable. It simply doesn’t work well for many. My CA 19-9 never got above 15, well below the upper limit of 37. Nonetheless, one area showing promise is genetic testing, but the development of a “predictive” test remains elusive.
My Diagnosis
An early detection test aside, I was one of the lucky ones. After a Friday lunch and feeling off over the weekend, I went to see my doctor, who ordered, as he called them, some “routine” tests.
To this day I’m not sure why I went to see him. Like so many guys, I thought I could tough anything out. Most often I would hunker down and wait for things to blow over. Had I chosen to do this, it would have been over for me. I would have become another sad statistic.
My doctor thought I might have a stomach bug or at worst C. diff, a bad bacteria in the gut. While I was waiting for my test results, the following weekend my condition got far worse. I spent that weekend with my stomach tied in knots and with waves of nausea crashing over me. Going back to see my doctor the following Monday, I asked, “Have you seen my test results yet?” To which he replied, “Dude, you’ve got other problems, you’re yellow!”
An emergency CT scan showed I had a blocked bile duct. During a procedure to insert a stent to open it, unbeknownst to me, they took a tissue sample. Two days later, the doctor who stented me popped into my hospital room and said, “I’m sorry, you have a malignancy.” Before I could muster a single question, he darted out the door. It devasted me that not even a doctor could say the C-word out loud.
Whipple Procedure and Its Aftermath
Perhaps once we have an early detection test in hand, funding should be redirected toward improving the difficult Whipple procedure, which was developed in 1935. Sadly, over the last 88 years, little has changed. Named after Dr. Allen Whipple of Columbia-Presbyterian Medical Center, it is considered one of the most challenging surgeries done. And it is so complex that only experienced surgeons attempt it. Depending on the expanse of the tumor, the head of the pancreas is removed along with the gallbladder and perhaps part of the stomach.
Not to be graphic, but with our pancreas buried deep within us, it is more like gutting fish. Worse, with these types of tumors often cementing themselves into our pancreas with their tentacles rooted like a weed into everything nearby, only one in five people are a candidate for a Whipple. Without it, death often comes within six months to a year.
My doctor compared it to open heart surgery. Talking with me minutes before my Whipple, he jokingly quipped, “When you wake up, you’ll feel like you got hit by a truck.” He wasn’t kidding. He should have added something about the truck being driven by a crazed maniac who would back up and run me over again for sport.
Although I had no choice but to go ahead with my Whipple if I wanted to stay alive, I had little idea how many complications would result from it and the follow-on radiation and chemo. After spending a month in the hospital after the procedure, I was sent home only to have my eight-inch incision open up, landing me in a wound clinic with a vacuum pump attached to me like a leech to help my incision heal. For two years, like clockwork every 8 to 12 weeks, I ended up back in the ER doubled over with stomach pain, and each time I was admitted for a few days until the pain subsided. The cause remained a mystery. Only after a massive infection spread from my pancreas into my left lung and then into my spleen did a gastroenterologist determine I had a tiny leak in my rebuilt pancreatic duct letting digestive enzymes ooze out inside me. Multiple stenting of the duct fixed this leak, and thankfully I haven’t had any more trips to the ER. This is not to mention that, like many with a third of their pancreas missing, I am now prediabetic. Courtesy of my radiation, osteoporosis set into my back, resulting in three very painful compressed vertebrae. Every six months, I get a Prolia injection. While this may sound like whining, it isn’t. Without a Whipple, despite how brutal I found it, and with complication on complication, I would not be alive. Surviving one is the first step to surviving pancreatic cancer.
More needs to be done to stop this killer. We should be embarrassed at how little progress has been made to crack this nut. Nonetheless, I remain thankful for the many excellent resources Let’s Win and its sister organizations provide. Whenever I come across yet another victim of this as part of my advocacy work, I always send them straight to Let’s Win.
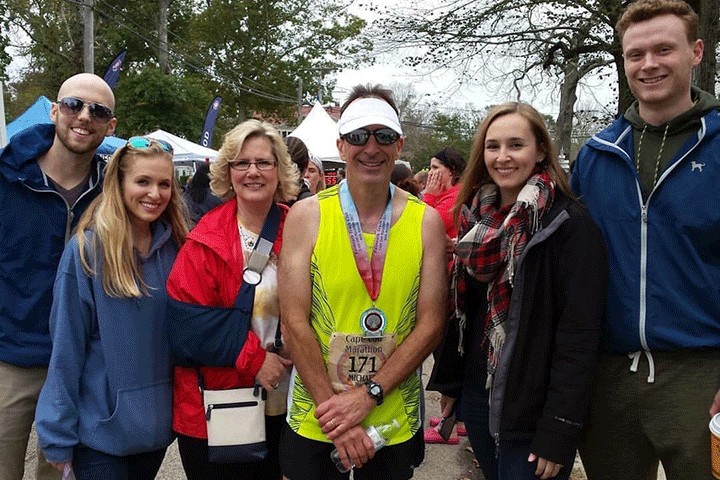
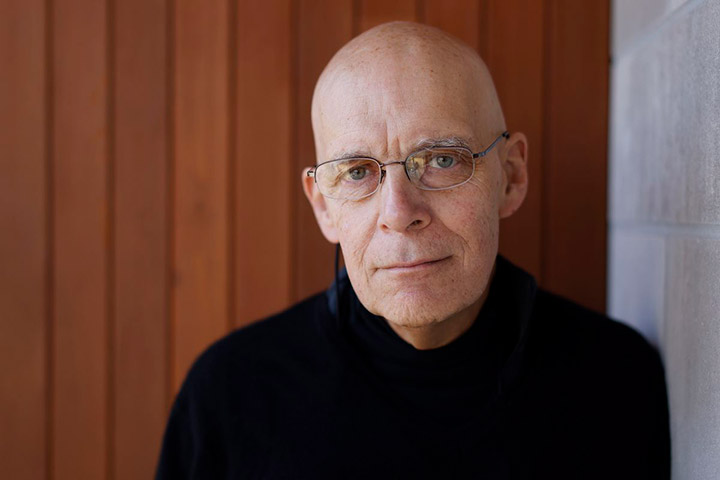
William Ramshaw lives in the expansive Pacific Northwest. He is a 10-year survivor of pancreatic cancer and has written a memoir, Gut Punched! Facing Pancreatic Cancer. He has written other stories and filmed a video for us.