Where Caregivers Can Turn When they Need Support

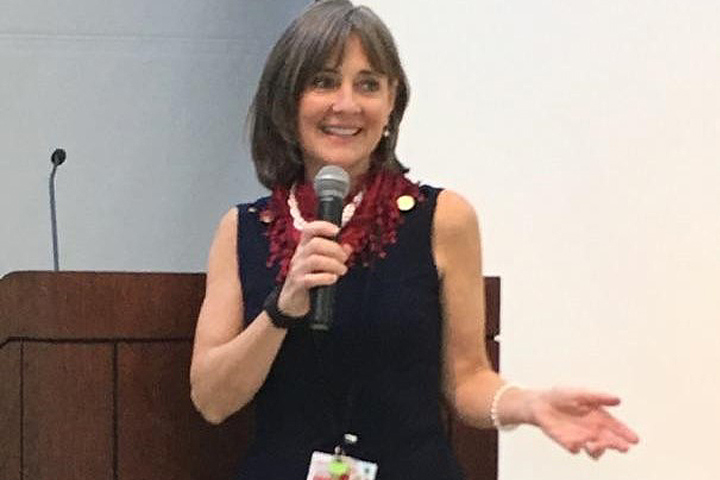
As a licensed clinical social worker who serves oncology patients and their families at Weill Cornell Medical Center in New York, Lauren Shaffer sees firsthand the stress and exhaustion that is common among caregivers.
“Most people aren’t prepared to shift roles all of a sudden and become a caregiver,” she says. “It’s taxing physically and mentally, and from an emotional standpoint it can be very overwhelming, very scary, and very challenging.”
With so much attention focused on the patient, it can be easy for caregivers to start neglecting their own needs. But it’s vital that they get support and make time for self-care, Shaffer says. “No one can caregive 24-7,” she says. “Nurses take a lunch break, they go home. But when a person is living with a patient, it’s all the time.”
Finding Caregiver Support Close to Home
For caregivers who are stressed or struggling, one of the best places to start finding help is within their own network of support providers, she says. A family member or friend can help the caregiver keep up with their own regular doctors’ appointments, schedule a check-up to make sure they’re taking care of their own health and are getting enough sleep, healthy food, and exercise.
Caregivers probably have friends and family members who’ve already reached out or offered to pitch in where needed, she notes. “Often they refuse the help or don’t tap into it because they think they should be doing those things themselves,” Shaffer notes. “They don’t want to put people out, or they don’t know what they need help with.”
If a friend has offered to help but left it open-ended by saying something like “let me know what you need,” caregivers can narrow down the offer by suggesting something specific, like driving the patient to chemotherapy, or picking up something at the pharmacy. Or if the caregiver is so overwhelmed that they don’t know what to ask for, they can ask the friend to suggest something concrete they’d be able to do.
One option if the patient is too sick to be left alone, is to ask a friend or family member to sit with them for an hour or two while the caregiver takes a break. “Many caregivers feel selfish going out and taking time for a yoga class, going for a walk, having coffee with a friend, but they desperately need that,” Shaffer says. “It’s self-care.”
Online resources like CaringBridge or Lotsa Helping Hands can make it easy to accept help and delegate tasks with tools like shareable calendars, where friends can sign up to deliver meals or provide transportation, she explains. So when a friend extends an open-ended offer of help, “you can just send them a link to the calendar.”
Tapping Into a Wider Network
In addition to friends and family, caregivers have an extended network of other resources they can turn to for support, Shaffer adds. Often, that starts in the hospital where the patient is receiving treatment, which can connect caregivers to a social worker, financial counseling, support groups, and other resources.
“It’s really ok to put your hand up and say, ‘Hey, I’m having a hard time, do you know who can help me?’” she says. “The oncology team will have someone on staff who can step in.”
If the caregiver or patient is employed, they can also look for support at work, Shaffer points out. Human resources departments can provide information about options like family leave, disability insurance, and financial relief programs; and many employers provide access to counseling or an employee assistance program (EAP).
Shaffer also refers clients to organizations focused on their type of cancer as well as general cancer organizations such as the American Cancer Society, which has caregiver guides and videos; and CancerCare, which helps connect caregivers with counseling, either in person, over the phone, or online.
Finding and attending a support group can also be extremely helpful, she says. It’s common for caregivers to feel isolated and alone, and to cope with feelings that people who aren’t in their situation may not understand, like frustration and even anger. “A support group is a wonderful place to be able to express that,” Shaffer says. “It’s a safe place where you can get support, not be judged, and feel some validation.”
If a caregiver lives in an area where in-person groups aren’t an option, or if it’s difficult to leave the house to attend a meeting, online support groups are another great option, she adds.
Making Time for Self-Care
While resources are available to give cancer caregivers much-needed support, for most people, the biggest challenge remains finding the time to use them. Rather than waiting for a window of free time that will never appear, Shaffer recommends that caregivers plan ahead and schedule time for rest and self-care, just like they schedule other appointments.
Each patient’s situation is different, so caregivers will have to think about their own schedule and what times are most likely to work. That could mean taking time to meditate first thing in the morning, before the day’s appointments begin; taking a break to read a book in another room when the patient is napping; or even going for a walk while the patient is in chemotherapy.
Online resources are also available for self-care, and Shaffer frequently recommends apps like Headspace or Insight Timer for guided meditation.
“Most caregivers have a calendar for all their loved one’s medical appointments. Some even keep detailed diaries of what their loved one eats, or how often they experience certain symptoms, sleeping schedules, etc.,” Shaffer says. “Yet it is not uncommon for caregivers to leave their own entries out of their calendar completely. It is important to block off some time and actually put it down in the calendar, whether it’s half an hour or an hour—and if you can make it daily, that would be great.”
While it can be hard for caregivers to find the time and energy to focus on their own needs, Shaffer says finding support needs to be part of the plan.
“You’ve got to put your oxygen mask on first before you save anyone else,” she asserts. “Remember that you’re going to take better care of the patient if you take care of yourself.”