Going the Extra Mile for Treatment—or Not?

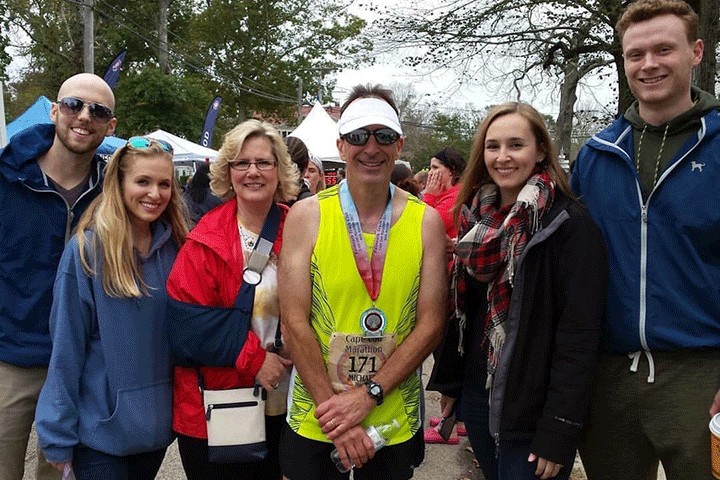
left: mhabegger1, Flickr; right: Chris Spielmann, National Cancer Institute
You’ve been dealt the diagnosis: pancreatic cancer. Now what?
Your family is pushing for the best possible treatment, advocating for a national cancer hospital or prestigious academic medical center. But you’d rather not have to travel to a big city for regular treatment.
The decision of where to seek treatment can be daunting, but it doesn’t need to be impossible. There are benefits to both community hospitals and academic centers, and it may even be possible to get the best of both.
Do Special Cancer Centers Equal Better Treatment?
To Karen Bird, the benefit of dedicated cancer centers is clear. “Unlike other hospitals, dedicated cancer centers exclusively treat cancer patients, with state-of-the-art therapies and research activities that often offer the greatest possibility for successful cancer treatment,” she says.
Bird is executive director of the Alliance of Dedicated Cancer Centers, a consortium of 11 institutions that are singularly focused on cancer–including the Dana-Farber Cancer Institute, MD Anderson Cancer Center, and Memorial Sloan Kettering Cancer Center—so is a cheerleader for science-driven comprehensive cancer care. “Much of the progress in understanding cancer’s biology and effective treatment is directly attributable to the work of our 11 centers,” she adds.
She is also able to point to some statistics that support her enthusiasm. Her organization commissioned an analysis of 46,762 Medicare fee-for-service patients who began receiving intravenous chemotherapy for treatment of breast, colon, lung, ovarian, pancreatic, or prostate cancer in 2010 and 2011 and were followed through 2014. The study found that patients treated at the dedicated cancer centers had a 17 to 33 percent lower risk of death within 36 months of starting chemotherapy than patients treated at other types of hospitals.
“Survival data is an important, but often missing, piece of information for cancer patients trying to make informed decisions about treatment options,” Bird explains. “When it comes to survival rates for some of the most common cancers, the type of hospital matters.”
The larger network of 70 NCI-designated cancer centers are also known for their expertise and capacity to treat all types of cancers, including rare and complex cancers. Along with academic medical centers, they may offer the widest variety of new therapies through clinical trials, and may be the only option for patients with certain cancers.
Is Smaller More Personal?
Christopher Sumey, M.D., agrees that expertise is essential when it comes to treating pancreatic cancer patients, especially those who are candidates for surgery. “A Whipple procedure is one of the most complex and involved surgeries a patient can be put through,” he says. “You want to be at a place where the surgeon has done a lot of them. Patients should absolutely feel empowered to ask their surgeon how many they do.”
Research published in 2017 supports claims that outcomes from treatment at “high-volume” hospitals—performing at least 15 to 20 surgeries per year—are better. But that doesn’t necessarily discount community hospitals.
Sumey is a medical oncologist at Sanford Health, the largest rural not-for-profit integrated health care system in the nation, with 45 hospitals and 289 clinics in nine states and three countries. Based at the Sanford Cancer Center in Sioux Falls, South Dakota, Sumey is one of nine medical oncologists and several other specialists treating thousands of cancer patients there each year. This includes about 50 to 75 new cases of pancreatic cancer, and about 20-25 surgeries, per year. “I have great confidence in our ability here,” he notes.
Not all pancreatic cancer patients are candidates for surgery, and the vast majority of all patients end up receiving chemotherapy. About half also receive radiation treatment. “You need to be at a place where there is a lot of expertise among the entire team, not just among the doctors, but among the nurses and other support staff who will be administering some of the treatments and helping you get through them,” Sumey says. “You should ask what kind of support there will be if anything goes wrong.”
Another benefit to being part of a local hospital network: Access to a wide range of medical services. Cancer can come with, or cause, related problems, such as pulmonary problems or diabetes. “No matter what other medical problems arise outside the clinic, excellent specialists are steps away,” he adds.
Sanford Health was one of the first National Cancer Institute’s Community Oncology Research Program (NCORP) community research sites, which means it served as an example of how to bring NCI-level cancer care into rural areas. It also means that the center—and its rural affiliates—continues to have access to a variety of clinical trials. It’s one of the things that drew Sumey to the center.
“We really do function like the larger academic centers, and rival many of the resources,” he notes. “We are able to offer the latest treatment options, and we are able to bring that close to home, so patients don’t need to travel.” There’s also enough of a community focus that patients don’t get lost in the shuffle, he adds.
“We’re always trying to find new ways of not only living longer, but living better. We really do know our patients here,” Sumey says. “Patients tell me that they still have the feeling of being appreciated as an individual. Knowing where our patients are coming from—both literally, in terms of geography, and figuratively, in terms of their life situations—makes us better able to tailor their care to best treat where they are at.”
By the Case
Otis Brawley, M.D., chief medical officer for the American Cancer Society, agrees that not all patients have to go the extra miles for quality care. As he told U.S. News and World Reports: “In commonly occurring diseases, and commonly occurring problems, we’ve got pretty good data to show that a community hospital and community doctor can do a very good job handling those things. And indeed, sometimes, can do a better job than a tertiary care facility.”
The dozens of chemotherapy nurses at larger hospitals might give a wide variety of treatments to many more patients, but be less intimately acquainted with the standard combinations you require, he said.
The convenience that community hospitals can offer should not be undervalued, he added. Patients often get through X-rays and other tests faster and spend less time waiting to see physicians, for instance. They may also be more likely to stick to their treatment regimen. An American Cancer Society study found that patients who have to travel farther to appointments are less likely to receive adjuvant chemotherapy (given after surgery to reduce the chance of the cancer returning).
For complex cases, however, Brawley suggested specialist centers or higher-tier hospitals. “Tertiary care centers tend to be much better in taking care of the out-of-the ordinary, unusual cancers,” he said.
Let’s Win has compiled a downloadable list of major teaching hospitals and cancer centers in every state of the United States, including many NCI-designated cancer centers. Not all of these facilities specialize in pancreatic cancer. Our partner Pancreatic Cancer Canada has provided a downloadable list of similar teaching hospitals and cancer centers in Canada.
Many local cancer centers are affiliated with major research centers, and you can receive excellent care at a local center which may be more convenient and closer to home.
This is an evolving list and suggestions are welcomed.