Radiation Therapy to Fight Pancreatic Cancer
Pancreatic cancer treatment is complex and almost always includes chemotherapy. But treatments can also include surgery and radiation.
With radiation, doctors use high-energy beams to shrink tumors in the pancreas. The beams create small breaks in the DNA of cancer cells to prevent them from growing and dividing. Just as the category “chemotherapy” encompasses many drugs, there are a number of types of radiation therapies, each with somewhat different effects. Each type is also used for specific reasons.
The Varying Roles of Radiation Therapy
Your treatment plan—whether chemotherapy, radiation, surgery, or some combination of those—depends largely on whether your tumor can be removed surgically.
If doctors can’t remove the cancer, patients are divided into two categories: Those who have locally advanced disease (meaning the cancer is largely confined to the pancreas and surrounding organs but has grown to include major blood vessels) and those who have metastatic disease (where the cancer has spread to distant organs).
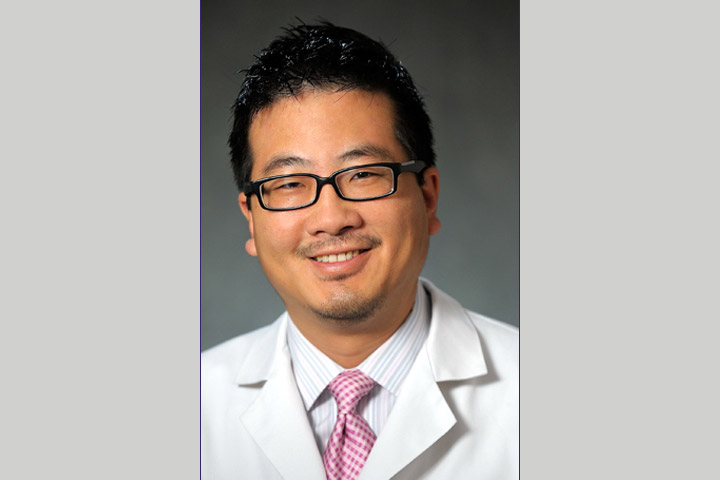
“By definition, radiation may be indicated for cancers that are localized in one spot,” says Dr. Smith “Jim” Apisarnthanarax, Associate Professor and Director of Radiation Oncology Clinical Research at University of Washington Medicine, and Seattle Cancer Care Alliance, Seattle. “When you have a cancer that has spread throughout the body, treatments that treat the whole body, like chemotherapy, become the focus of treatment, and localized treatments like radiation become less important.” But that doesn’t mean there isn’t a role for palliative radiation in patients with advanced metastatic disease.
Radiation can be a tool for both situations. Here’s how it breaks down:
Curative: Even with curative approaches, doctors may add radiation before or after a chemotherapy regimen. “If a patient has localized cancer that the surgeon can’t remove, we start with chemotherapy for four to six months. If there is still concern that the surgery can be done safely or if cancer may be left behind after surgery, that’s when radiation may have a role,” says Apisarnthanarax. In some cases, radiation helps the tumor shrink enough so doctors can remove it. Patients may also receive radiation after surgery and adjuvant chemotherapy, to kill any microscopic cancer cells that were left behind at the surgical site.
Stall progression: Radiation therapy may help delay progression for patients whose tumors are confined to one particular area. While scientists don’t know whether radiation improves survival rate, studies show it can help prevent the cancer from growing locally. “Some people have outstanding benefit from systemic chemotherapy followed by radiotherapy,” says Apisarnthanarax. And when patients become eligible for surgery after chemotherapy and radiation, they can have prolonged survival—often as long as patients who came in with a resectable cancer.
Palliative: Doctors often use radiation not to cure cancer, but to relieve symptoms and enhance patients’ quality of life. “Say, for example, a pancreatic cancer tumor is bleeding or putting pressure on the stomach such that food cannot go through, and the patient can’t eat or throws up soon after eating. We can use radiation to address that issue by focusing the beam on the area of tumor involvement,” explains Apisarnthanarax. Radiation can also help relieve problems such as pain or difficulty swallowing.
Types of Radiation Therapy
The most widely used radiation therapy for pancreatic cancer patients is external beam radiation. In this technique, a machine outside of the body directs a beam, or multiple beams, into the body to reach the tumor site. But there are a few different key approaches:
3D Conformal Radiation Therapy (3D-CRT): 3D conformal radiation therapy allows doctors to use three-dimensional scans to get images of the tumor before delivering radiation beams. So instead of using a “flat” 2-dimensional x-ray, doctors rely on advanced imaging, such as CT or PET scans, to clearly define the tumor and normal organs in three dimensions. Then doctors use computer software to ensure radiation beams deliver an optimal dose of radiation to the tumor while sparing healthy tissue.
Intensity-Modulated Radiation Therapy (IMRT): Like 3D conformal radiation therapy, IMRT relies on three-dimensional imaging, but uses sophisticated computer systems to precisely shape many beams of radiation, sculpting the radiation to treat the tumor. Since IMRT is more precise, doctors can often use higher doses of radiation without damaging the surrounding tissue. So, if a tumor is wrapped around an artery or pressing on healthy tissue, IMRT can shape the radiation to steer clear of those structures.
Stereotactic Body Radiation Therapy (SBRT): Like IMRT, SBRT delivers radiation from several beams to target radiation even more precisely, typically to smaller-sized tumors. Since the treatment is so targeted, patients’ breathing and abdominal organ movements need to be tightly managed, so customized devices that either limit or minimize these motions may be required. Because it’s so precise, doctors can give patients large daily doses over just a few treatments. Unlike 3D-CRT and IMRT, doctors typically give SBRT without simultaneous chemotherapy.
Currently, there is no definitive evidence that SBRT is better than other forms of radiation for pancreatic cancer. Research is ongoing to determine what role SBRT has in the treatment of pancreatic cancer.
Proton Beam Radiation: This type of radiation relies on proton beams rather than photon beams, which are delivered with 3D-CRT, IMRT, and SBRT. As opposed to photons, where the radiation energy is deposited within the body and also exits the body, protons are charged particles that deliver most of their energy at the tumor site with little to no exit dose beyond treating the tumor. This allows for less radiation to be delivered to surrounding normal tissue so that it could possibly translate to decreases in side effects. “We don’t have definitive data proving that protons are any better than photons for pancreatic cancer treatment,” Apisarnthanarax says, “but we do have some evidence that suggests that using proton beam radiation after surgery may possibly reduce side effects.”
Ablative SMART Radiotherapy: A new type of precision radiation therapy, called Stereotactic MRI-guided On-table Adaptive Radiation Therapy, or SMART, is showing tremendous promise for pancreatic cancer patients. Two companies, Denver, Colorado-based ViewRay Technologies, Inc. and Stockholm, Sweden-based Elekta offer MRI-guided linac (linear accelerator) systems that integrate MRI imaging with a linear accelerator, allowing doctors to image and treat patients simultaneously.
The MRI produces high-quality images in real time during treatment while the linear accelerator remains focused on the tumor, targeting it with high-energy radiation beams. With this two-pronged approach, the system tracks tumor position, and if it moves outside of the target range, to pause radiation delivery until the tumor returns to position. The end result: Targeted treatment with fewer side effects. In fact, preliminary studies on pancreatic cancer patients show a two-year overall survival rate of more than 50 percent, double the expected two-year rate of 20 percent with lower-dose radiation.
Radiation Side Effects
The experience of getting radiotherapy is similar to getting an x-ray, but with a much higher dose of radiation. The procedure itself is painless, but as with any therapy, it does come with side effects.
“During treatment, you might feel nauseous and fatigued. You may experience diarrhea and vomiting,” explains Apisarnthanarax. You may also lose your appetite and notice changes in your skin. Usually side effects go away within a few weeks of completing treatment. Unfortunately, a subset of patients will suffer from lower blood counts and increased risk of infection. In rare cases, they may also develop some complications months or years after treatment is completed, such as intestinal bleeding.
In every case, careful planning can help you sidestep serious side effects. Your best defense: Talk to your healthcare team, not only about the goals of radiation treatment, but also about how to best weather treatment.