Being Persistent Led to my Cancer Diagnosis

- Stage IIIb pancreatic cancer
- Tumor wrapped around an artery
- Chemotherapy plus radiation and a clinical trial at Johns Hopkins
- Modified Appleby procedure
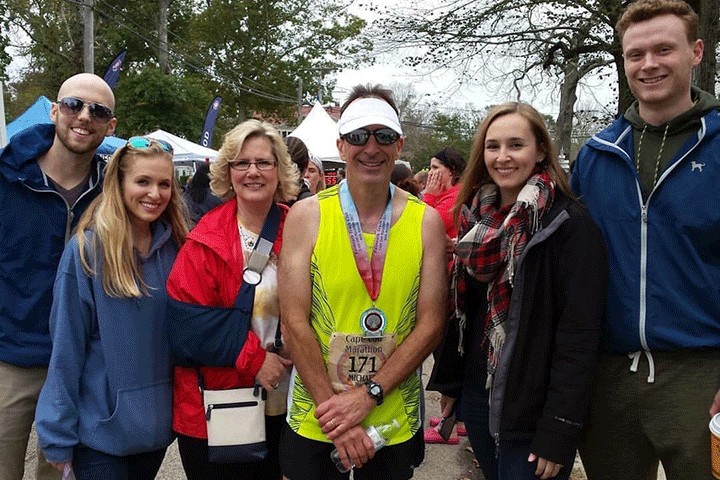
I was a long-distance runner for six years when I was diagnosed with pancreatic cancer. Like most of my runs, my pancreatic cancer journey has been long.
Mine began in 2016 when I ran the Richmond Half Marathon. In the process, I worsened an existing hernia. By December of that year I needed surgery to repair not one, but three hernias! I resumed running again in January 2017, but started having minor lower back pain.
My back pain worsened over time and I also developed abdominal pains, which I believed were adhesions from the hernial repair. I returned to my surgeon, who reported that there were no adhesions and the hernias were healing fine. The pain must be caused by something else.
That same year, I got remarried, to someone I had known since high school. That was a bright spot among an otherwise difficult period of my life. My pain continued and I became a regular visitor at my general practitioner (GP) and six other specialists, including an orthopedist, a neurologist, and several pain management doctors. I sought relief with multiple physical therapists, chiropractors, and a massage therapist. I even bought a new mattress. I was surviving each day with over-the-counter painkillers, but nothing truly alleviated the pain or allowed me to sleep at night. By the end of the year, the pain was constant and debilitating.
Finally Getting a Scan
In early 2018, my digestive issues began. They were disruptive to my personal life—sometimes when my wife and I were out having dinner, I would rush to the bathroom before I finished my meal. By March I had lost 30 pounds. I was calling my gastrointestinal (GI) doctor every week and seeing my GP constantly. By the end of April, I presented a journal of my illnesses to my GP. He ordered a CT scan even though he was skeptical that anything would be found. But something was found. That’s when we discovered the tumor on my pancreas.
In the year leading up to the discovery, no one had ever mentioned pancreatic cancer. I was shocked and devastated. Within a week of the diagnosis I had a biopsy, which led to surgery to insert a nerve block. Unfortunately, my lung was punctured during the procedure, which landed me in the hospital for an extra three days. My GI doctor referred me to a colleague at Richmond’s Virginia Cancer Institute (Dr. David Trent, now retired) who would take direction from Johns Hopkins, where I wanted to have surgery.
Once released, I went to Johns Hopkins for testing and to meet the multidisciplinary pancreatic cancer team. The team included Dr. Ana De Jesus-Acosta (oncology), Dr. Jeffrey Meyer (radiology), Dr. Richard Burkhart (surgery) and others. At that time I was confirmed to be stage IIIb but would have probably been stage IV within a couple of weeks. More bad news: The tumor was wrapped around an artery, which rendered me ineligible for surgery at that time.
Treatment and Emotional Support
I began a treatment of FOLFIRINOX chemotherapy, with morphine for my pain, in June 2018. My wife reported the news to our circle of friends via social media and asked them for prayers. More than 200 people and a dozen church lists were praying for me. It was uplifting to know that my life and well-being were in so many people’s thoughts. I used this time to focus on pancreatic cancer success factors and stories. Thinking positively was the only way forward.
My chemo treatments continued for seven months. Luckily, the side effects of the treatment were minor. By December the tumor had shrunk, so I moved on to intense radiation at Johns Hopkins for five consecutive days. I also participated in a clinical trial for a pancreatic cancer vaccine from December 2018 through January 2019.
Modified Appleby Procedure
By February 2019 I was deemed a good candidate for surgery. Dr. Burkhart at Johns Hopkins was planning a modified Appleby, a technique that removes two-thirds of the pancreas, the spleen, and the celiac axis. There were risk factors. For instance, if the surgical team found that the cancer had spread to my liver, the surgery would stop. Also, I could develop stomach complications, diabetes, and even die during the procedure. Despite the risks, I only wanted to know how soon they could operate. I was all in.
I had the modified Appleby procedure on February 28, 2019. It took six and a half hours. They removed most of my pancreas, spleen, 17 lymph nodes, and my celiac axis. The surgery was a success! The margins were clean and I was released a week later with no complications.
I left the hospital with a Jackson-Pratt drain inserted into my abdomen to take care of the excess fluid. I was also put on a no-fat diet. I thought that I would starve to death! Once the drain was removed two months later, I was able to slowly increase my diet. Now I can eat almost anything in moderation—except chocolate, onions, and foods high in fat.
By June 2019 I was back on FOLFIRINOX as a precaution. This time it completely drained my energy. I also ended up with pneumonitis (a noninfectious lung inflammation). As a result, I was not able to continue with the vaccine clinical trial. I was disappointed.
Living a New Normal
Fast forward to March 2020 when I completed a 10K at Belle Isle State Park. This was one year post surgery. Believe it or not, I finished first in my age group! (Note: I was the only one registered in my age group!) I was so happy and proud to be back on my feet again.
Around that same time, my scans detected some spots growing in my lungs. In June 2018 the doctors at Johns Hopkins had concluded that these spots were caused by my punctured lung and were not cancerous. However, my CA 19-9 stats started to go up, which was cause for concern. In May 2020 I started gemcitabine (Gemzar) and paclitaxel (Abraxane) for seven months. I had many side effects from this combination, including fatigue, chills, mouth sores, and foot, ankle, and leg swelling.
I stopped chemo from November 2020 to April 2021, and then started again with Gemzar and capecitabine (Xeloda). I developed mouth sores again and my hands began to peel—it was unbearable. The Xeloda dose was decreased, which made it more tolerable. I have been stable for about a year with only neuropathy in my hands and feet. My oncologist believes that I will be on and off chemo for the rest of my life.
Giving Perspective to Others
I tell everyone to maintain a positive attitude because “Attitude is half of everything!”
Before it all started, I never questioned what a doctor said. Now I have learned that if you aren’t satisfied with what a doctor tells you, get a second or even a third opinion. You must advocate for yourself.
Being in good physical condition was key for me to tolerate the past four years of treatment. I turned 73 in 2022 and took my health for granted before my diagnosis. My advice is to get as much exercise as your doctor will allow. But also listen to your body—if you need to take a nap, take it! At the same time, maintain your diet, eat healthy, and avoid stress. Also, be careful what you read on the internet. A lot of data is incorrect or out of date.
Finally, I believe in the power of prayer. My favorite acronym “PAAPA”—prayer and a positive attitude—can help you cope with a lot!