Learning to Recognize the Symptoms of Pancreatic Cancer

- Long-term stomach troubles lead to pancreatic cancer diagnosis
- Whipple surgery and chemotherapy
- Radiation treatment
- Educating others on symptoms and risks
At the end of 2011 or beginning of 2012, I had an acute episode of vomiting and watery diarrhea that lasted eight hours, through the night.
This was after consuming three glasses of red wine and a pasta dish with bacon bits. I felt better the next morning and because I was taking care of my elderly mother who had had a stroke, unfortunately I did not go to the hospital or to the doctor for some time.
Even before this episode I had been having abdominal pain and health issues, and they continued after. I had what has been diagnosed in retrospect as pancreatitis in 2010-2011. I was diagnosed with a fatty liver early on, around 2011. I had a history of falling due to the pressure on the nerves around the pancreas. I had changes in stool in 2013-14 due to pancreatic issues. I took Zantac for a number of years because of heartburn. I had severe itching on and off for some time. I made numerous visits to gastroenterologists without ever getting a definitive diagnosis. In 2019 I had severe crippling back pain due to the undiagnosed tumor. I had all these symptoms, but nobody seemed to be able to recognize them as related to each other.
Fast forward to March 2020. On two consecutive days I went to walk-in clinics in Los Angeles. The first doctor gave me Cipro for a stomach bug. The second doctor took my urine and said my bilirubin was high. He took my blood and sent me home, later sending me a note saying, “Nothing serious, come back for a scan.” But when I looked at my chart the next day it included a report of highly elevated labs that proved to me that I needed immediate treatment at the emergency department instead. On March 28, 2020, I was seen at the UCLA emergency room for fatigue, jaundice, vague stomach pain, and itching in my heels and shoulder blades that was ongoing but had worsened after receiving Cipro from the first visit to a walk-in provider.
An Answer to Years of Suffering
I am a true warrior, having suffered for years with an array of signs, symptoms, and risks. After 20 minutes in the ER, I knew I had adenocarcinoma in the head of the pancreas—stage T2N0.
I had jaundice and a bile blockage which was temporarily fixed with a stent. More testing showed moderately to poorly differentiated pancreatic cancer. I learned this while I sat alone, with my husband waiting in the car due to COVID-19. The cell service was not working in the basement where the ER was located, so he sat there for five hours without knowing what was happening. We never expected to be on this journey, especially after three recent cross-country car trips to visit California. Luckily, I was in the right place at the right time where my broken pieces could be fixed.
Whipple and Chemotherapy
My open Whipple surgery was done at Hoag in Newport Beach by Dr. Maria Stapfer (now at Providence in Fullerton), who has performed over 1,200 Whipple surgeries. About 10 days in I developed an abscess in the surgical area. Several months later I developed three hernias by the incisional area. I had my first course of chemotherapy with gemcitabine at a senior (lower) dose. After several treatments I had a reoccurrence in the peritoneum and the spleen. My chemotherapy was switched to capecitabine at my request because I felt the former drug did not stave off the disease. The peritoneum and spleen cleared of the cancer, but after about a year of the oral chemotherapy, I had another reoccurrence, this time in the mesentery (the folded membrane that connects the intestines to the abdominal wall).
I wanted hernia surgery as my hernias were rapidly growing, likely faster than the cancer. My doctor asked for a biopsy of the mesentery. After some negotiations we agreed to both. In April of 2021, my hernias were repaired with mesh, doing open surgery over the previous incision.
In August of 2021, I had a reaction to my oral chemotherapy where I developed diarrhea and then crippling back pain. This happened just weeks before I started radiation therapy. My back pain was dramatic, and I visited the emergency room three times for the pain. I was scheduled for five high-dose radiation treatments averaging one and a half hours each for the mesentery tumors, starting September 21st and ending October 1st. I almost skipped the last treatment because the back pain was still a problem. Instead, I took some powerful pain killers and completed my last dose, bringing a box of donuts to help the staff work faster. There was never a diagnosis on the back pain, but it cleared after a dose of antibiotic for a possible urinary tract infection.
Waiting for My Results
My next PET scan is in January 2022, when I will see the full effect of my treatment. I wait to hear the results. I asked the radiologist about possible success of the treatments, but he was unable to tell me with any certainty. I feel much of what we take for treatment is still early in terms of knowing the outcomes.
I tried the Xcures food study, a preclinical trial, but that I was unsuccessful in staying on that diet because of my food preferences. There were powdered protein shakes included and they were too bitter to drink. It is hard enough to eat real food as chemotherapy alters the taste of everything.
I had genetic testing of every tumor and biopsy but only one mutation—of the Mutyh gene—was found. This has not influenced my treatment plan and it didn’t appear to be a factor in pancreatic cancer.
I moved to Thousand Oaks, California, in August of 2019, after seven years in the state of Virginia. However, I am a native New Yorker, where I hold many of my memories of living there for 59 years. I feel that I am alive at 66 years old today because of the good doctors in California who have given me the best care possible. I am currently under the care of UCLA and see my oncologist, Dr. Sidharth Anand, every three weeks. He is very knowledgeable and always takes my needs into consideration before making any decisions. He is supportive and encouraging, always offering hope. This is the most important element in the process of recovery.
Educating Others
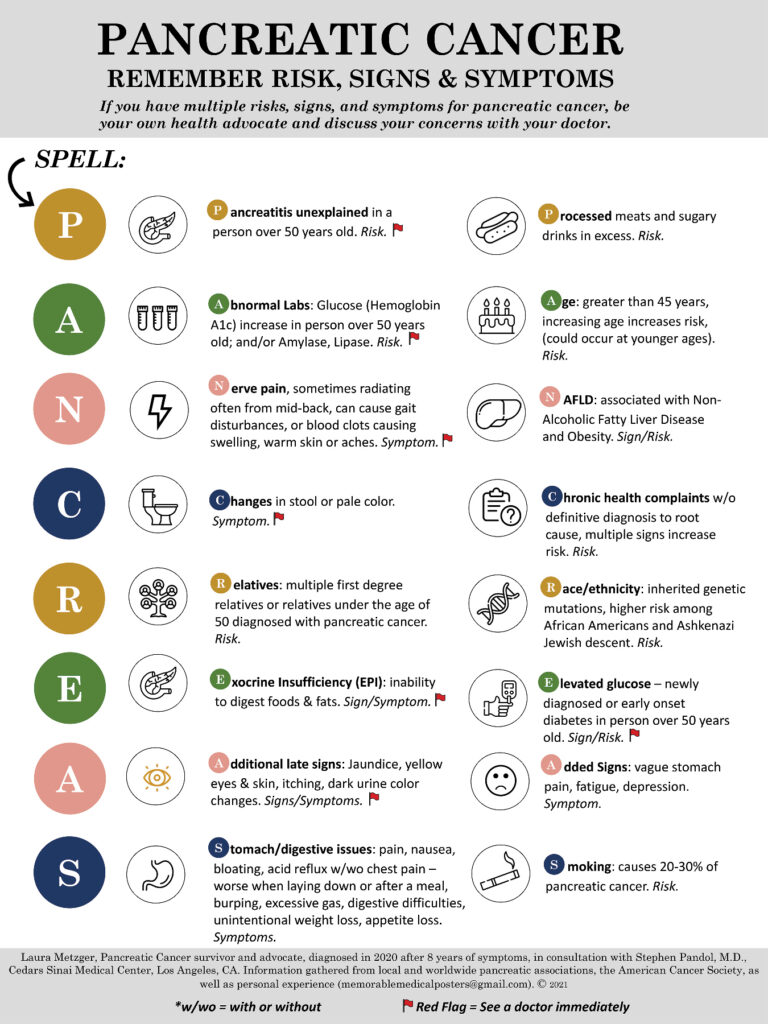
I have worked with Dr. Stephen Pandol, a researcher at Cedars Sinai (Los Angeles), for the past year and a half to create a poster that shows the signs, symptoms, and risks of this deadly disease. Our goal is to improve early diagnosis through an educational tool that is memorable for doctors and patients. This will be revised yearly as new facts become available. Please use the attached poster for your clinics, doctor offices, and where appropriate.
Almost two and a half years after her diagnosis, Laura passed away from pancreatic cancer. For the pancreatic cancer community her legacy is the poster she designed to raise awareness of the symptoms of this disease. We offer our deepest condolences to her family.