A Cancer-Free Life 25 Years in the Making
- Family history of pancreatic cancer
- Annual screenings lead to early diagnosis
- Distal pancreatectomy surgery
- FOLFIRINOX chemotherapy
Pancreatic cancer has taken far too many of my loved ones away from me: my grandmother and at least two of her sisters; my mother, her twin sister, and their brother; and finally, 25 years ago, it took my brother’s life.
It’s been a devastating journey to watch all of this unfold. But I didn’t want to follow that same path. After I lost my brother, I made it my life’s mission to not only avoid the same fate, but to help find a way of stopping the pancreatic cancer killer in its tracks.
Finding a Specialist Was Key
After my brother passed away in 1998, I started seeing a local oncologist for annual pancreatic cancer screenings. If I was destined to get it, my goal was to catch it early. I was so naïve then. I thought cancer was just cancer but I soon learned not all cancers are the same. Pancreatic cancer was a monster all of its own, and I realized the oncologist I was seeing didn’t have a lot of experience with it. He was well-versed in other types of cancer but not pancreatic cancer. In those days, there wasn’t a lot of research on pancreatic cancer or many effective treatment options.
I wanted a specialist who knew pancreatic cancer inside and out. I found Dr. Randall Brand and knew he was the right one for me. Not only was he a pancreatic cancer specialist, but he was also conducting research on pancreatic cancer that runs in families like mine.
I was living in Des Moines, Iowa, at the time (I still do) and Dr. Brand was in the process of moving from Omaha to a hospital in Chicago. When you find the right doctor, the distance doesn’t matter. I met with him in Chicago to learn about his study and to see if I would even qualify to be part of it.
He began by asking me a series of questions about my family history. I only needed to answer the first two questions about common genealogical factors before I was accepted into the study: Does my family have a history of pancreatic cancer? Am I of Eastern European Jewish descent? The answer to both questions was “yes.” He immediately invited me to take part in his research project, which would include a routine of annual endoscopic ultrasounds to check out my pancreas, collecting tissues and secretions, and blood and genetic testing, all to help with early cancer detection.
After a few visits to Chicago for testing, Dr. Brand told us he was relocating to the University of Pittsburgh Medical Center Shadyside (UPMC) and hoped that wouldn’t be a deterrent to my continuing to participate in the study. That wasn’t even a question in my mind. I strongly felt then as I do now: He is the one I need to be with. I very strongly believe in him and his research. Why mess with a good thing?
I have had an annual screening every year since then, except for one year that I skipped during COVID. Our persistence paid off.
The Diagnosis Was Not a Surprise
Following my annual endoscopic ultrasound in October 2021, Dr. Brand said that cancer had shown up on my scans. By then we had developed a strong personal relationship and it was as emotionally difficult for him to tell me the news as it was for me to receive it. With my family history, the diagnosis really came as no surprise. I knew it was coming. As shocking as it was, I knew I was in the right place to deal with it.
One silver lining is that my cancer was diagnosed early. Very early. I had no symptoms and if a stage had to be given to it, I’d say it was barely stage I.
Two days later, I met with surgical oncologists Dr. Amer Zureikat and Dr. Alessandro Paniccia at the UPMC Hillman Cancer Center, who said the tumor was in its infancy and that complete removal would not be a problem. The additional silver lining was that the procedure would be done robotically, which made it less invasive and could result in a faster and easier recovery.
I have always been a positive thinker. I was diagnosed early and had a team of the best medical providers on my side. Not only that, pancreatic cancer research and treatments have come a long way over the past 25 years. I remained determined to get through this and truly had no doubt that I would.
Surgery and Chemo
Ten days later, on November 15, 2021, Dr. Paniccia performed the surgery: a robotic-assisted distal pancreatectomy and splenectomy, plus a celiac axis lymphadenectomy.
I spent a week of recovery at the hospital. I then spent another 10 days at a local hotel to further recuperate and to attend follow-up appointments. Thanksgiving fell right in the middle of that time. Dr. Brand invited us to spend it with his family at his home. It was perhaps the best Thanksgiving ever. I had a lot be thankful for then. And being there with them made it ever so meaningful.
A week later my wife and I returned home to start twelve rounds of chemo with Dr. Thomas Buroker at John Stoddard Cancer Center at UnityPoint Health. My treatment was what I like to call a chemo cocktail: FOLFIRINOX, comprised of oxaliplatin, fluorouracil, irinotecan, and leucovorin. This chemo was considered a preventative measure just in case a cancerous cell or two had floated away to plan another attack. My docs were taking no chances.
The chemo caused side effects including an intense sensitivity to cold, some hair loss, peripheral neuropathy in my hands and feet, cloudy chemo brain, constipation, and loss of appetite. I didn’t have any nausea or diarrhea, often associated with this chemo—and I was thankful for that.
Once my chemo was done, I went through six months of chemo rehab, which included physical therapy to help regain balance and occupational therapy for my hands. During those sessions, the therapists used ultrasound to help with the neuropathy in my feet and hands. I also did three months of acupuncture for the neuropathy. The other side effects gradually went away.
I’m participating in a personal training class for cancer survivors to improve strength, mobility, and balance. It’s offered through Iowa-based Above + Beyond Cancer, a terrific organization that offers various free programs to elevate the lives of cancer survivors as well as those who have been touched by cancer.
I had my one-year follow-up appointment in November 2022. Dr. Paniccia found no trace of cancer in my body. His exact words were, “I see nothing to worry about. Go. Live life. You’re cancer free.”
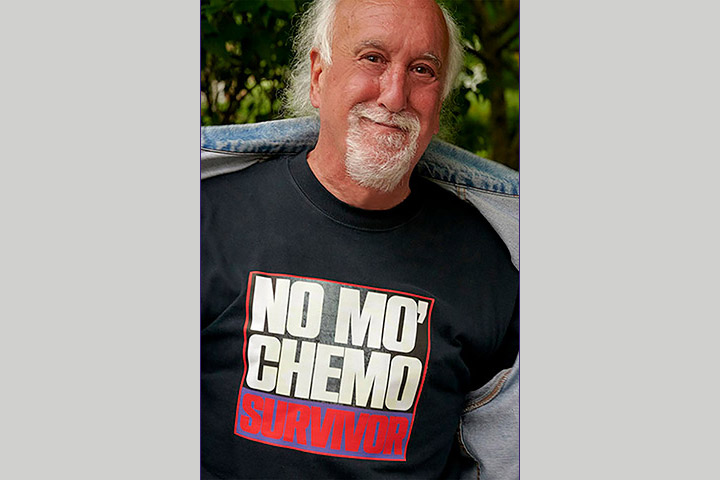
While I still have some neuropathy, it is definitely better. Did any or all of the treatment for it make a difference? Probably, but I think time helped greatly. Today I am 15 months out of chemo and living and loving my cancer-free life.
My 30-year mission to stop this pancreatic cancer killer will continue. While I’ve had a number of genetic tests, my family’s genetic link has yet to be discovered. I’m fully confident that one day it will be. Until then, I’ll be heading back to Pittsburgh every October for routine scans.
Early Detection Can Save Your Life
Whether or not pancreatic cancer or any cancer runs in your family, get checked out. Early detection can save your life, just like it did for me.







