At a Crossroads for Pancreatic Cancer Treatment
- Diagnosed by chance after a colonoscopy
- Chemotherapy plus vitamin D and an antimalaria drug
- Continuing treatment controls the cancer
I find myself at a crossroads. A decision needs to be made regarding my continued treatment for pancreatic cancer.
My story began in September 2016 when I was 75. I had a routine colonoscopy which lead to one test after another. After a CT, MRCP, EUS-FNA, and PET scans, I was informed that I had a 2 cm tumor on the head of my pancreas and that the cancer had spread to some lymph nodes.
My first meeting with my oncologist, Dr. Muhammad Abbasi (Mountain Lakes, New Jersey), was in early December 2016. He recommended that I be treated with FOLFIRINOX. I wanted a second opinion of my prognosis and what needed to be done, so I scheduled a consultation with Dr. John Chabot of Columbia-Presbyterian in New York City. Two days after my initial meeting with him, he performed a laparoscopic biopsy of my abdomen and found cancerous lymph nodes. He confirmed that I had stage IV adenocarcinoma, and that the tumor could not be surgically removed.
Starting Chemotherapy Treatment
My first chemo treatment was on December 30, 2016. I went through six cycles of FOLFIRINOX followed by a CT scan that yielded disappointing results. In May 2017 we changed to the GAX regimen (Gemzar, Abraxane, and Xeloda) with a schedule of two weeks on and one week off. In June 2017, we supplemented the GAX with infusions of Zemplar three times a week. Zemplar (paricalcitol) is a synthetic form of vitamin D which Salk Institute researchers found to “collapse the barrier of cells shielding pancreatic tumors, making this seemingly impenetrable cancer much more susceptible” to chemo drugs.
At the end of 2017, we dropped the Xeloda, which was causing rashes. We added daily hydroxychloroquine (HCQ) tablets to my treatment. HCQ is designed for the prevention and treatment of certain types of malaria. HCQ is believed to interfere with a cancer cell’s internal processes, inhibiting its ability to function.
I have since learned that Zemplar and HCQ are being tested in some clinical trials. A discussion of their use on another patient—Dr. Stephen Bigelsen—was featured in a Conquer magazine article in October 2018.
I continued to use this combination of drugs through August 2018. By that time the tumor was reduced to nondetectable on CT scans, and my CA 19-9 levels were in the 20s and 30s. Dr. Abbasi recommended that I go on a maintenance dose of chemo, getting the same drugs but reducing the frequency to every other week. I continued having the Zemplar infusions and the HCQ tablets as before. Six months later Dr. Abbasi reduced the Zemplar infusions to twice weekly.
During the course of my treatment, I periodically arranged for consultations with doctors in the New York area who have expertise with pancreatic cancer. Not all were proponents of Zemplar and HCQ, but since the drugs didn’t seem to cause any harm, they never suggested that I stop using them. In September 2019, I had a PET scan and the radiologist reported a “complete metabolic treatment response,” meaning that no cancer was found. In October 2019 I met with Dr. Allyson Ocean of Weill Cornell Medicine (New York),who, after noting my overall progress, recommended that I take a “chemo holiday” to allow my body to recover. She also suggested that I continue to take Zemplar and HCQ, due to their possible therapeutic effects, even without the chemo.
At a Crossroads
I discussed Dr. Ocean’s recommendation with Dr. Abbasi. I’ve been receiving chemo for three years and by January 2020, I will have received 87 separate infusions. The chemo is wearing me down—anemia, fatigue, and neuropathy are the obvious symptoms, but there are probably other things going on with some of my organs that I should be concerned about. Stopping or curtailing chemo has its risks too. Will the cancer recur? And if so, will resuming chemo control it once again?
During a December 2019 visit, Dr. Abbasi recommended that I cut back, but not stop, the chemo. Our plan is to stop the Abraxane and to continue with the Gemzar. Abraxane is the most likely cause of my neuropathy. We will monitor my cancer markers and CT scans closely, and if the cancer recurs, the Abraxane will be resumed. In the future it may be possible to stop the Gemzar as well.
My cancer treatment has been surprisingly successful. However, there have been many challenges along the way. Although I am not going to go into too much detail, since being diagnosed with cancer I have experienced many different medical issues. Problems such as Lyme disease, cataracts, sciatica, or a kidney stone were not related to my pancreatic cancer treatment. But my other issues included a three-week hospital stay, intestinal obstruction, infection with Clostridium difficile bacteria, Bell’s palsy, four endoscopic retrograde cholangiopancreatographies (ERCPs) with three stent placements, unpredictable and explosive bowel issues, port replacement, pulmonary embolism, inferior vena cava filter installation, neuropathy, and blood transfusions,.
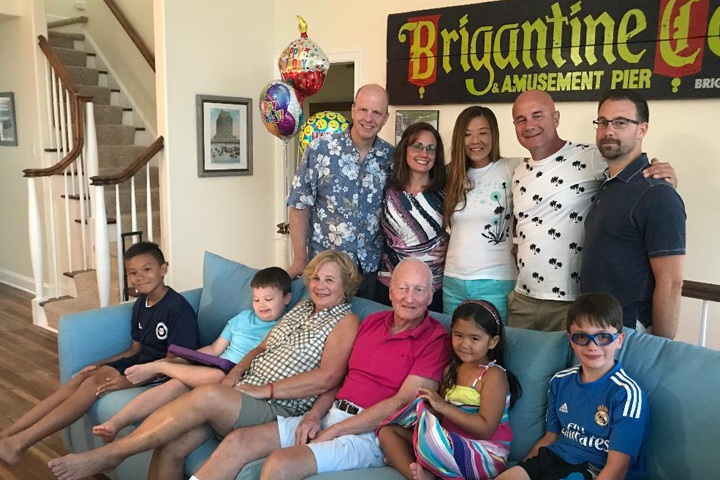
But with help from my superior medical support team, moral support from family and friends, and a lot of luck, I have overcome or been able to tolerate these conditions, and for the time being, we have the cancer under control.
Ed passed away after an almost four-year battle with pancreatic cancer. He pursued the latest treatments, and we appreciate that he shared his story with Let’s Win. We offer our deep sympathy to his family.






