A Clinical Trial Matches My Genetics
- Whipple surgery
- Conventional chemotherapy with Gemzar but the cancer spreads
- FOLFIRINOX shrinks the tumors
- Clinical trial with PARP inhibitor halts the disease
In mid-June 2012 at the age of 55, I was diagnosed with pancreatic cancer.
The symptoms I experienced prior to visiting Dr. Daniel Goldin, my physician, were subtle. I first noticed a bit of fatigue in the last week of April of that year. I had a very long commute from my home on the Jersey Shore to my job in Manhattan, so I thought perhaps I needed to get more rest on the weekends.
By mid-May I noticed a darkening of my urine; by Memorial Day weekend I was experiencing gastritis when eating. That weekend was a turning point. It was perfect beach weather, yet I had no desire to go to the beach—I was happy inside my home doing assorted projects. I knew something was not quite right.
When I got to Manhattan on Tuesday morning, I decided to see my doctor before going to my job at the research lab. I was in luck—Dr. Goldin was able to squeeze me in. I described my symptoms and he took my vitals and did a routine urinalysis. Everything was within the normal ranges. He suggested I give it till Friday to see if the symptoms would resolve. I returned on Friday feeling no worse but not feeling any better either. I had blood work done and planned to return Monday for results. But when I got home Friday evening I noticed that the whites of my eyes looked yellow. I looked at the underside of my forearms and noticed the skin had a jaundiced appearance as well.
Monday morning I returned to Dr. Goldin, who immediately got me an appointment for an ultrasound to check for gallstones or other blockage of the bile duct. The ultrasound was negative, but he called Brian Turner, M.D.—a hepatobiliary surgeon at Weill Cornell Medical Center—and scheduled an immediate appointment.
Finally, a Diagnosis
The surgeon performed an endoscopic retrograde cholangio pancreatography (ERCP) to determine the source of the blockage. Dr. Daniel Cherqui, the chief of surgery of the department, inserted a stent to dilate the biliary duct, which allowed bile to drain out and enter the intestine. After the procedure he informed me that the blockage was due to a cellular mass in the pancreas. The good news—I was eligible for Whipple surgery. Dr. Cherqui wanted to operate immediately because of the aggressiveness of this type of tumor. We agreed the operation could be scheduled for the following Monday morning. Since I live alone, I needed the time to get personal affairs in order and arrange for post-surgical support by family and friends.
I took the news of my diagnosis of stage IIb pancreatic cancer calmly. My first thought was that my family and friends would not believe what I would be telling them. They knew I ate healthy since my teen years and did frequent 50-mile bike rides for speed and endurance. There were instances of breast and colon cancer on the maternal side of my family. Because of this, my mother set an example by exercising, eating healthy, and dealing with adversity in a calm, rational manner. I assessed my situation and formulated a plan of recovery and recuperation. I was fully aware of the seriousness of my diagnosis and was determined and focused on being a long-term survivor.
Whipple Surgery Followed by Chemotherapy
Whipple surgery was performed on Monday, June 18th and took over 9.5 hours. During my recovery I learned of the unexpected finding that the tumor was projecting onto the hepatic artery and vein. This added complication resulted in the procedure taking four additional hours. After a convalescent period of two months, I began conventional chemotherapy with Gemzar. A CT scan was performed after 12 sessions, to assess its effectiveness. The result was not encouraging. A total of six small tumors were found—two each in three of the four lobes of the liver. This led to a re-classification of stage IV for my cancer.
Dr. Manish Shah, my oncologist immediately switched me from Gemzar to the more potent cocktail FOLFIRINOX. After 12 cycles on the new regimen, the corresponding CT scan revealed significant shrinkage of the tumors.
Genetic Testing Leads to a Clinical Trial for PARP-1 Inhibitor
Because of my family history of breast and colon cancer, I did a more thorough investigation and found out that three of my relatives with cancer were known to be positive for the BRCA gene deletion. My own test revealed I was positive for the BRCA-2 gene deletion. Studies have shown that BRCA-positive individuals have a very good response to platinum-based chemo drugs. I then met with Dr. Steven Lipkin, a geneticist, who informed me of a new class of drugs that were showing promise with the BRCA gene defect.
I searched the Internet for clinical trials testing PARP-1 inhibitors, and located an article presented at a scientific symposium that was published a few days earlier. The Pancreatic Cancer Action Network helped me with contact information for the lead author, Dr. Susan Domchek, executive director of the Basser Center for BRCA at the Hospital of the University of Pennsylvania. I met the clinical criteria and was accepted into the trial. I began taking the PARP-1 inhibitor a few weeks after finishing a treatment cycle of the traditional drug cocktail I was on. I showed a positive response to treatment with the PARP-1 inhibitor and I continue taking the drug to this day.
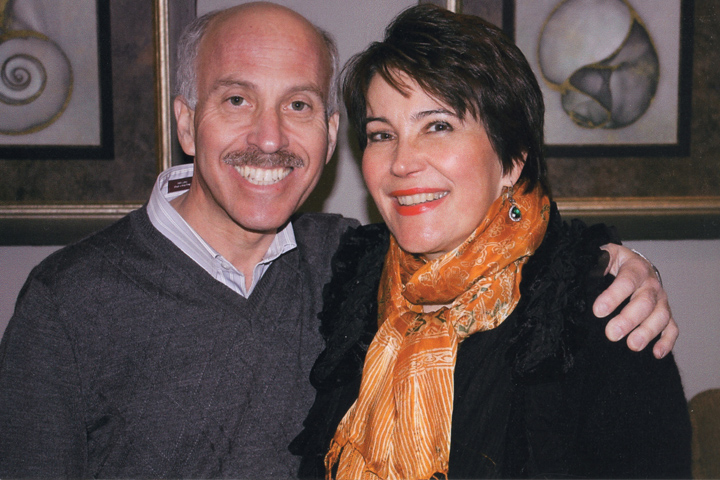
I am now nearing the five-year anniversary of my Whipple surgery. The tumors that can be seen on scans have significantly decreased in size. I remain stable with no sign of spread or new disease. During my conventional chemo treatments, I became involved with mentoring medical students. Additionally I speak to cancer patients about my story—what I did to improve my health, staying focused, and instilling hope in others.
Steven shares more of his story in the Survivors video “Plenty to Live For.”