Collaborative Multi-Center Immunotherapy Trial Targets CD40 and PD-1
Pancreatic cancer researchers are finding ways to out-think deadly pancreatic cancer cells by using new techniques in molecular biology and immunotherapy.
The good news for patients is that this research is quickly moving out of the preclinical stages in the laboratory and being brought to clinical trials. Equally important is the ability to rapidly get information back to the laboratory to fine-tune aspects of clinical trial care, depending on what early data may show.
Bench to Bedside and Back
That ability to quickly move from bench to bedside and from bedside to bench is just one of the important aspects of a new, multi-center phase I/IIb trial for metastatic pancreatic cancer using combination chemotherapy and two immunotherapy agents, explains Dr. Mark O’Hara, who is the principal investigator leading the efforts at University of Pennsylvania’s Abramson Cancer Center. The main purposes of this study are to learn how safe and effective the study drug combinations are in treating patients with metastatic disease. The drug combinations are APX005M (from Apexigen) plus nivolumab (brand name Opdivo, from Bristol-Myers Squibb) plus gemcitabine and nab-paclitaxel, or just APX005M plus gemcitabine and nab-paclitaxel.
“There are actually two very good things about this study,” says O’Hara, who is also an Assistant Professor of Medicine, Hospital of the University of Pennsylvania. “The first is that it is one of the more aggressive front-line trials in the country that has strong scientific rationale from preclinical mouse data. Second, moving from bench to bedside is always important, but being able to get back to the bench is vital. We are collecting blood samples and tumor biopsies throughout the trial, and that will give us the ability to quickly learn who this may or may not benefit and help us adapt future clinical trials. In other words, we are going to be able to answer the ‘who,’ ‘why’ and ‘why not’ questions more quickly and potentially get solutions more quickly, too.”
Making Immunotherapy Work for Pancreatic Cancer
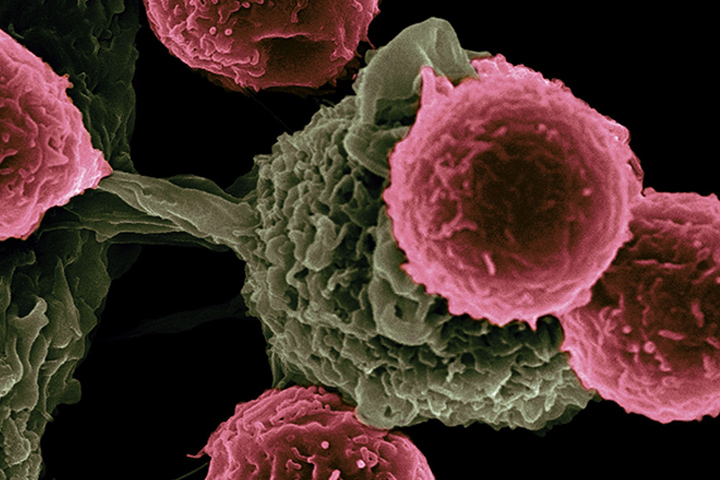
While immunotherapy has shown incredible promise in cancers such as lung cancer or melanoma, it has been less effective in notoriously immune-resistant pancreas cancers. However, in this trial, researchers hope to tackle pancreatic cancer’s immune-resistance with a one-two punch consisting of two immunotherapy agents.
The immunotherapy agent APX005M is a monoclonal antibody, which is a type of protein made in the laboratory that can bind to substances in the body, including cancer cells. APX005M targets the protein CD40. Once activated, CD40 can spur the immune system to attack cancer. The other immunotherapy agent, nivolumab, is a type of immunotherapy called a checkpoint inhibitor. Checkpoint inhibitors block certain proteins made by some types of immune system cells, such as T cells, and some cancer cells. Nivolumab targets and blocks a protein called PD-1 on the surface of T cells. Blocking PD-1 activates the T cells to find and kill cancer cells.
The trial is a collaborative effort of the Parker Institute for Cancer Immunotherapy and Cancer Research Institute, Bristol-Myers Squibb, and Apexigen. The research will be conducted across the Parker Institute’s network of cancer research centers, which includes the Abramson Cancer Center of the University of Pennsylvania, as well as University of California Los Angeles, University of California San Francisco, Stanford University, University of Texas MD Anderson Cancer Center, and Memorial Sloan Kettering Cancer Center. The goal is to recruit approximately 105 patients.
“I am really excited about this because this is a great first step to getting more of the answers that we need,” says O’Hara, who co-designed the study with the overall study principal investigator, Dr. Robert Vonderheide, director of the Abramson Cancer Center, and one of the nation’s leading experts in pancreatic cancer, the CD40 pathway, and immunotherapy. “And, hopefully, we are going to be able to help patients who desperately need more effective treatments for this disease.”