Reopening America: Guidelines For Pancreatic Cancer Patients
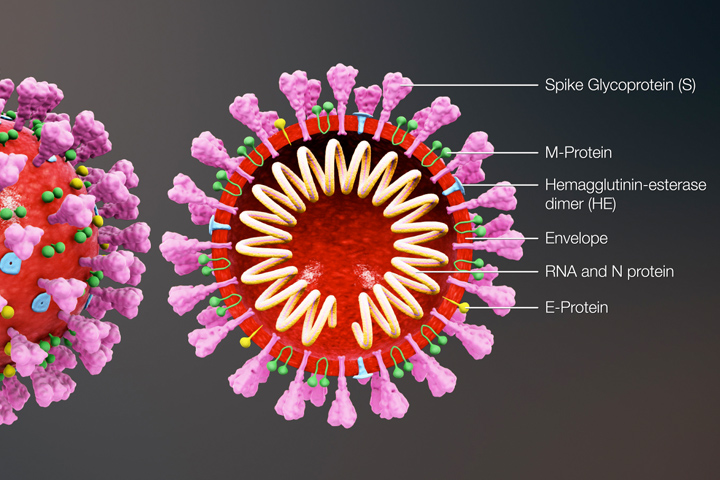
As of May 19, 2020, more than 1.5 million people in the U.S. have been diagnosed with COVID-19, and more than 91,000 Americans have died in the pandemic.
These numbers are still climbing every day, even though mitigation efforts to “flatten the curve” have been successful in many areas of the country. Lockdown and quarantine have been effective in the hardest-hit areas, but the U.S. economy has been decimated, with more than 36 million jobless claims filed. Some jobs and businesses may never come back. That’s the scenario government officials face while trying to reopen various nonessential businesses that have been closed for more than two months. It’s a seemingly untenable dilemma: how to keep people safe while trying to restart state economies.
Many health experts say that reopening too soon will decimate any gains made in trying to control the spread of COVID-19. States are still trying to expand testing and set up contact tracing (tracking people who came in contact with someone who had the virus). Better treatment options are needed and, of course, a vaccine for prevention.
Many people have “quarantine fatigue” and are desperate to get out of their homes, go to a restaurant, see their families and friends, and return to some semblance of normalcy. But if you have pancreatic cancer or love someone with the disease, that so-called normalcy was disrupted at diagnosis. Your life changed prior to COVID-19.
We are all well aware that cancer patients, especially those undergoing active treatment, such as chemotherapy, are immune-compromised. Cancer patients, especially those with metastatic disease, have greater risks and face poorer outcomes from COVID-19, according to research. So, if your state is opening up, are there ways for pancreatic cancer patients to safely get out more often?
Talk to Your Team and Don’t Become Complacent
The very first thing you should do is talk to your medical care team about your risk, says Dr. Allyson Ocean, of the NewYork-Presbyterian Hospital/Weill Cornell Medical Center and Associate Professor of Medicine at the Weill Medical College of Cornell University. “Every patient is different, but what I’m telling my patients, in general, is that you should continue to stay home, whenever possible,” she says. “COVID-19 has not disappeared.”
Although “flatten the curve” is usually an epidemiologic term, it has become part of our lexicon. It’s important to remember what it means, says Ocean, who also serves as chair of the Let’s Win Scientific Advisory Board. “The goal of flattening the curve was to slow the spread of COVID-19 so that fewer people would need to seek treatment at any given time,” she explains. “That’s why there were stay-at-home recommendations, nonessential business closures, social distancing, and recommendations to wear masks.”
“We have flattened the curve, but we are not out of the woods. We all need to protect ourselves and, as a physician caring for cancer patients, I want to make sure my patients don’t become complacent about risks from this virus. The risks are still there and very real.”
Her recommendation now is the same as it was a few months ago: Limit outings to necessary ones. Even better, use delivery services or curbside pickup. Although it is less risky for a friend or family member who is living with you to do essential errands, every time that person goes out, they are at risk of contracting the virus and bringing it back home. “Depending on where you live delivery services may be overwhelmed or even unavailable, so I understand that not every cancer patient in the U.S. is going to be able to use these kinds of services,” Ocean acknowledges. “The message is if it’s available, try to use these kinds of services. If not, do the very best you can to minimize risk.”
Depending on where you live, parks and beaches may be reopening. And although in general open air, uncrowded environments are by their very nature safer than closed, crowded environments like a bar or restaurant, there is still risk. “There can be surfaces in public restrooms or concession stands that you may touch,” Ocean says. The way to minimize that risk is by frequent hand washing or sanitizing. And, of course, stay at least six feet away from others, and wear a mask, which can reduce person-to-person viral spread and serve as a visual reminder not to touch your face and to keep your distance, she adds.
Living with pancreatic cancer is not easy. Living with pancreatic cancer during a pandemic is even harder. That’s why it’s very important to be good to yourself. “Pancreatic cancer and COVID-19 aren’t fake diseases,” notes Ocean. “They are real threats and it’s absolutely normal to be scared. Take a break from worry and try to find something that takes your mind to a better place. Read a book, watch some TV, have a Zoom get-together with friends and family. Most of all, know that you are not alone.”
Phased Reopening and Vulnerable Individuals
The White House recently unveiled Guidelines for Opening Up America Again. It is a three-phased approach, based on the advice of public health experts, for individuals, employers, and businesses, including office settings, gyms, restaurants, bars, and more. The plan is to have states move through these phases as they meet certain thresholds. For full details you can read the entire document.
According to the White House guidelines, during Phases One and Two of reopening, vulnerable individuals should continue to shelter in place. Members of households with vulnerable residents should be aware that by returning to work or other environments where distancing is not practical, they could carry the virus back home. Precautions should be taken to isolate from vulnerable residents.
Vulnerable individuals include elderly individuals as well as those with serious underlying health conditions, including high blood pressure, chronic lung disease, diabetes, obesity, asthma, and those whose immune system is compromised, such as by chemotherapy for cancer and other conditions requiring such therapy. In Phase Three, vulnerable individuals can resume public interactions, but should practice physical distancing, minimizing exposure to social settings where distancing may not be practical, unless precautionary measures are observed.
The CDC has released a series of separate reopening guidelines for schools, workplaces, child care programs, mass transit systems, youth programs and camps, and restaurants and bars. Each guideline is set up as a decision tree, where the choice of whether to open or not, and at what level, depends on the answer to a question. The decision trees are based on state, local, and federal guidelines for hygiene, social distancing, and monitoring. The CDC has also release a full document giving extensive guidance on reopening.
It is also recommended that individuals continue to adhere to state and local guidance as well as complementary CDC prevention information, particularly with respect to face coverings.