This Is What It’s Like To Live With Pancreatic Cancer

Anne Glauber, 62, a Manhattan-based PR consultant, was feeling sluggish 2 years ago when she was diagnosed, shockingly, with stage 4 pancreatic cancer. Thanks to pioneering doctors willing to try experimental treatments, she’s living life to the fullest. Here’s what it’s like to be living with the fourth most deadly cancer.
In May 2014, I happened to make an appointment with a dermatologist for a regular skin check. I was feeling well—I had no symptoms of any disease. I was enjoying my work as a public relations manager and had just written and published a book. I was a little tired, but my husband reassured me. “You’re juggling so much, of course you’re tired,” he said.
Before the dermatologist looked at anything else, he held up a mirror to my face. I gasped. My eyeballs were very yellow. He told me to see my doctor right away to get blood tests to figure out why I was jaundiced.
The blood tests were followed by a sonogram and a CT scan, and 5 days later my life was completely and totally transformed. The CT scan results were sent to a surgeon who specialized in pancreatic procedures. My children, my husband, and my brother all came to the appointment with me. “I have a devastating diagnosis to give you,” the surgeon said. It was stage 4 pancreatic cancer, and he thought I had less than a year to live.
He told me I had two chemotherapy options available. One had bad side effects, and the other was worse. Neither would give me much more than an additional month to live. That was how he left it with us; he was pretty brusque. We left the appointment completely stunned, totally shocked. Everything changed in that appointment. My reality was shattered.
I didn’t want to spend the time I had left being sick from treatment. I had no signs or symptoms other than feeling tired—it wasn’t like I was in pain. So everyone in my family got to work. We researched reputable doctors, pancreatic cancer specialists, and what kind of interesting and innovative research was happening in the field. There wasn’t any central place to go online for this information; it was all fragmented and difficult to find. Luckily, I was able to connect with two expert doctors in pancreatic cancer treatment who are willing to take science-based risks to integrate experimental research into their treatment plans.
I flew out to Los Angeles to be treated for a month by William Isacoff, M.D. Most pancreatic cancer patients are put on one of two treatments, and the awful reality is those treatments don’t work in the long run. Initially, treatments can stabilize the growth of the cancer, but after a while it just stops working. Plus, the side effects can be really uncomfortable and difficult to manage. Dr. Isacoff provided smaller doses of chemotherapy over longer periods of time, so I’m able to tolerate treatment better. Since I live in New York City, Dr. Isacoff recommended Allyson Ocean, M.D., and I’ve been seeing both doctors ever since. The fact that both are willing to go beyond the standard of care in pancreatic cancer has made all the difference in my treatment.
My doctors were willing to introduce me to other scientists in the pancreatic care community because of my treatment experience. I connected with scientists doing really interesting experimental work, which my doctors integrated into my treatment even though it’s not yet validated by a clinical trial. Getting a sense of what these scientists are working on has helped me understand what heroes they really are.
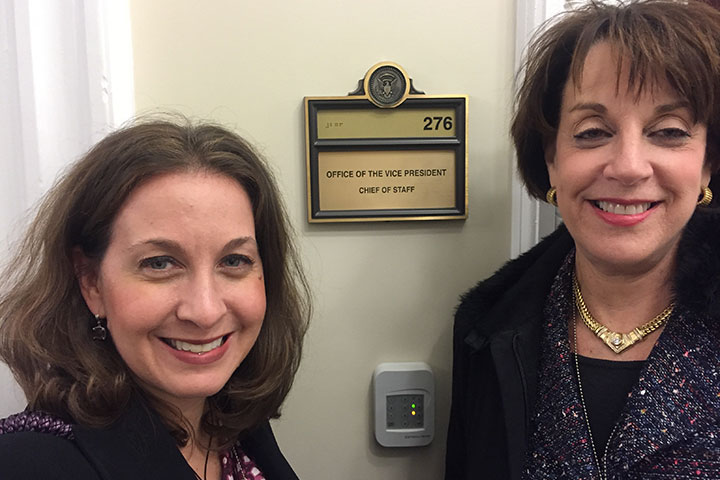
But I wanted other patients to have access to this incredible work, too. In May 2016, I launched Let’s Win, a pancreatic cancer online community. I wanted to provide a place where patients could share their own experiences as well as highlight promising science and connect patients with scientists and clinical trials in their area. I get comments and emails from patients thanking me for starting Let’s Win. I feel we are really making a difference for patients who have few options.
Because that’s the reality of pancreatic cancer. It’s scary; it’s always on my mind. It’s the first thing I think about in the morning, and the last thing I think about before I go to sleep. But it helps to work on a day-to-day basis with incredible people devoting their time to helping other people with this disease. It’s not discussed as much as breast cancer, and yet almost 42,000 Americans will die from pancreatic cancer in 2016. More people are diagnosed every year.
The American Cancer Society reports that pancreatic cancer has a 29% survival rate 1 year after diagnosis and a 7% survival rate after 5 years. I appreciate life every day. I receive treatment for 2 weeks and then I’m off for 2 weeks. My treatment has changed every 3 to 4 months over these 2 years. It keeps on changing because my tumors keep on mutating. The cancer cells are extremely clever and figure out how to defend against a specific type of chemo that has been given for a while. Every 6 weeks I have blood tests to determine how my tumors are changing and what chemo will have the strongest impact on them next. I can feel tired from treatment and sometimes have an upset stomach, but the side effects are not debilitating.
I am more comfortable thinking about things in the short term. It’s easier for me to live with this diagnosis when I am thinking month to month. It sounds prosaic to say, but being diagnosed with pancreatic cancer makes you really live in the present. Thankfully, every day I’m out and about living a full life.
This article was originally published on Prevention.com on October 5, 2016.