Listen to Your Body

- Discomfort leads to pancreatic cancer diagnosis
- Genetic testing shows a BRCA mutation
- Treatment with FOLFIRINOX and a change of treatment centers
- Whipple and other surgeriesA
In November of 2012 I was diagnosed with stage III inoperable pancreatic cancer.
Starting in August, I noticed a loss of appetite and an intermittent pain under my left rib cage. I also had been having low back pain for a couple of months, which I thought was from driving—I was an account executive for an environmental service company covering the Southeast—so I didn’t even think about my back. Although I had breast cancer in 2002, I was very healthy and physically active.
When I saw my internist in September, she thought the pain was due to the fact that I drove about 800 miles a week. I should have emphasized that the loss of appetite would have nothing to do with my driving, but of course I wasn’t at all thinking I could possibly have pancreatic cancer. That would be a death sentence, so my mind didn’t even fathom thinking about such a dreadful disease.
My internist checked my pancreatic enzymes and they were normal. She then encouraged me to see my OB/GYN to check my left ovary (the right one was removed in the early 1980s due to a solid cyst) and a gastroenterologist to schedule a colonoscopy, to see if the pain could be GI related. I thought for sure I probably had a polyp or diverticulitis. Eight weeks later I returned to my internist for a follow-up on my hypothyroidism and high blood pressure. I had seen the GI PA and was scheduled for a colonoscopy at the end of November, but I had not seen the OB/GYN. I told my internist that I was still having pain, only now I had stomach issues and had lost more weight. She immediately ordered a CT scan. Two days later, on November 16, 2012, she called me to confirm that the scan revealed a lesion on the tail of my pancreas.
A Dreaded Diagnosis and Genetic Testing
My internist arranged an appointment for me with a local general surgeon who had a lot of experience with the Whipple surgery. I saw Dr. Bing Yi in Greenville, South Carolina, the next week and he immediately discerned that although my lesion was small it was inoperable because it involved an artery. I had an MRI and then an EUS to biopsy the tumor, in order to confirm it was cancer. The plan was to have life-saving chemotherapy that would shrink the tumor away from the artery and make surgery possible.
The EUS confirmed that I had an exocrine tumor called adenocarcinoma, the most common kind of pancreatic cancer. At this time, I also underwent genetic testing since my only risk factor was that I was 60. I never smoked, was not overweight, and did not consume sugary drinks. The genetic test showed I was BRCA2 positive; this explained my previous breast cancer as well as my pancreatic cancer.
Let the Chemo Begin
I began treatment at St. Francis Cancer Center the first week of December. But I wanted a second opinion, as I knew I only had a 5 percent chance of surviving five years. After my first two chemo treatments, I called Cancer Treatment Centers of America. A representative steered me to CTCA’s Tulsa, Oklahoma location. Within two weeks I was at CTCA in Tulsa to meet with my care team, which included oncologist Sagun Shrestha. I also had my fourth FOLFIRINOX treatment while I was there. The initial plan was to have six chemo sessions—one every two weeks and then a PET scan to see if the tumor was now operable. But I had a scan while I was in Tulsa, and found out that the tumor had shrunk so much that it looked like I had already had surgery. My tumor was now operable. Unfortunately, I still had positive abdominal lymph nodes so I still had to undergo the six rounds of FOLFIRINOX.
As part of my treatment I was offered acupuncture, a naturopathic doctor, a registered dietitian, a masseuse, a psychologist, and pastoral care. All of these were important to me and helped with my treatment and side effects. Even though I was having the same chemo back home in Greenville, I decided that I would have the rest of my treatment at CTCA Tulsa, because they treat the whole person and not just the disease. The acupuncture helped with fatigue and stress. One of the side effects of the chemotherapy was a very low platelet count. The naturopathic doctor recommended special drinks and supplements to help with this and other side effects, such as neuropathy in my hands and horrible mouth sores. There was only one time I had to wait an additional week for my chemo infusion due to a low platelet count.
On June 25, 2013 I completed my 12th round of chemotherapy. In July I went back to Tulsa for a PET scan to determine if I could finally have the 10-hour sub-Whipple surgery. My son Matt came with me and to our surprise there was no evidence of disease. NED is the acronym that is every cancer patient’s aspiration.
Time for Whipple Surgery
Surgeon Pierre Greeff (now retired) told me that he would need to meet with the tumor board to decide if I could undergo the 10-hour surgery. The consensus was that because I was a fit and otherwise healthy 61-year-old, my best chance of survival was surgery. So on September 25, 2013, my sister Renee came to Tulsa to be with me while I underwent the 10-hour surgery that would remove 60 percent of my pancreas, all of my spleen, left ovary and fallopian tube, my left adrenal gland, and the omentum (the covering of my stomach).
Because of my BRCA2 mutation Dr. Shrestha recommended that I undergo a proactive complete hysterectomy. In November of 2014 I had that surgery in Greenville, with Dr. David Godwin. He was shocked to get my biopsy results, which found a precancerous polyp on my uterus. He was very pleased that my oncologist had recommended the surgery as I was heading for uterine cancer. I continued to have PET scans every three months at CTCA Tulsa; my scans remained clean. In 2014, I volunteered for Cancer Fighters with CTCA, to tell recently-diagnosed pancreatic cancer patients about my successful treatment.
Dr. Shrestha also suggested that I have a double mastectomy because of my BRCA2 mutation. So in late February 2015 I underwent a double mastectomy with reconstruction; because of complications related to my previous breast cancer treatment, the whole procedure was not completed until a year later in 2016.
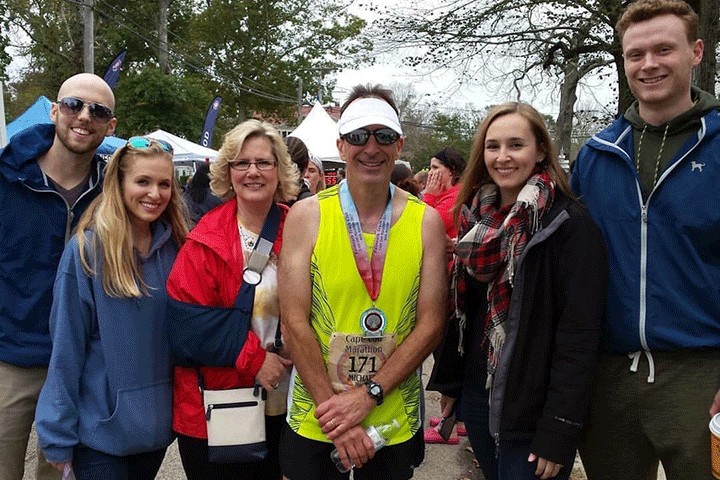
Finally, Life Without Surgery
In the summer of 2016 I was finally able to return to playing golf. I was quite rusty, but I have worked my way back into shape. I also started working part-time with a senior care organization in February 2017. I love my clients and find the work very rewarding and not stressful. I celebrated my five-year pancreatic cancer survival with a 12-day European river cruise, a trip of a lifetime. I am a thriving pancreatic cancer survivor. Life is good!
Watch Roxanne tell her story in “The Optimist.”