CRISPR-Engineered Immunotherapy for Metastatic GI Tract Cancers
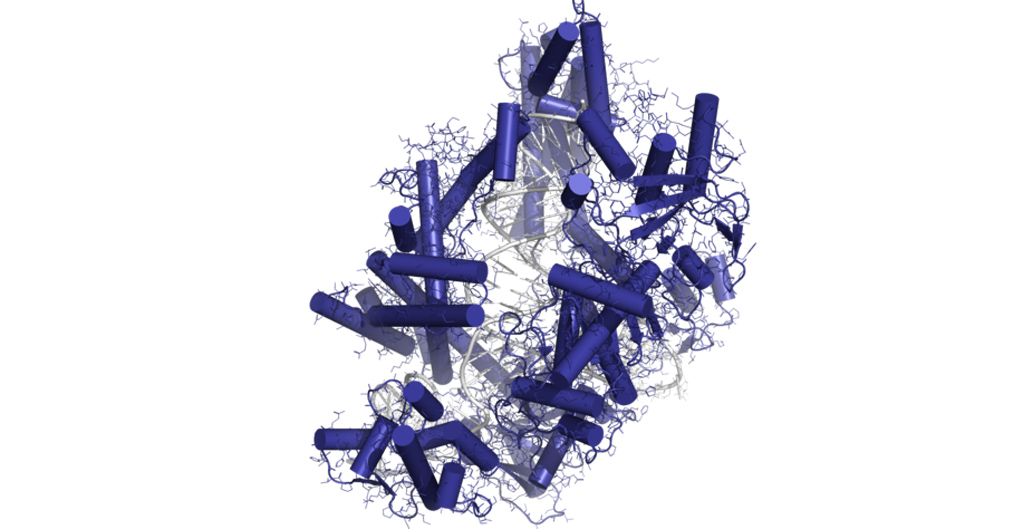
Elena I Leonova; Wikimedia Commons
Could gene-editing technology be used to target a previously undruggable checkpoint inhibitor and provide the first engineered T cell therapy for metastatic gastrointestinal cancer?
Researchers are using CRISPR gene editing to delete the CISH gene in certain types of T cells to enhance their ability to better target and destroy tumors of patients with metastatic pancreatic and other gastrointestinal cancers.
What is CRISPR?
CRISPR is a type of gene editing technology that gives scientists the ability to add, remove, or alter the genetic material of an organism at specific locations in the genome. The CRISPR technology has generated a lot of excitement in the scientific community because it is faster, cheaper, more accurate, and more efficient than other genome editing methods.
What Is CISH?
The cytokine-inducible SH2 (CISH) gene encodes the CISH protein, which interferes with the signaling of T-cell receptors. CISH acts as a checkpoint inhibitor that is believed to play a key role in preventing T cells from recognizing and eliminating tumors. Because CISH is expressed inside the cells it is not easily druggable with more common molecules such as a cell surface-targeting antibody.
The purpose of this clinical trial is to inactivate CISH in tumor-infiltrating lymphocytes (TILs) and other T cells to augment their ability to target and destroy solid tumors. In order to do so, CRISPR gene editing technology will be used to delete the CISH genes in T cells harvested from trial participants. The engineered cells lacking the CISH genes will then be reinfused back into trial participants.
A Multi-Step Trial
The trial begins with surgery to remove pieces of the tumor. The T cells are extracted from these tumor pieces, grown out in the lab and subjected to CRISPR-mediated knockout of CISH.
Next, participants will have chemotherapy with cyclophosphamide, which interferes with DNA replication so the tumor cannot grow, and fludarabine, a medication used to treat leukemia and lymphoma, which inhibits DNA synthesis in cells and is often used with cyclophosphamide. The purpose of this treatment is to reduce the patient’s own T cell numbers, so they will not later interfere with the proliferation of the infused engineered T cells.
Once the engineered cells have been expanded in lab culture, they will be reinfused back into the patient, along with the immunotherapy drug aldesleukin, an immunotherapy drug that stimulates the body to fight cancer. The phase I/II trial will measure the maximum tolerated doses and the safety of the modified T cells, as well as the preliminary effectiveness of the treatment.
Who Can Participate
All participants must have metastatic gastrointestinal epithelial cancers (including gastric, liver, pancreatic, and colorectal cancer) that have not responded to first-line standard therapy. The trial is based in Minneapolis, Minnesota. Because of the nature of the trial participants must be able to stay in Minneapolis for at least a month.
We encourage you to consult your physicians for clinical trials that may be right for you. The website ClinicalTrials.gov provides more details about this trial as well as many others. You can visit the Let’s Win Trial Finder for a list of all active pancreatic cancer clinical trials.





