Frequently Asked Questions About Pancreatic Cancer

You or someone you love has just been diagnosed with pancreatic cancer.
You have questions but don’t know where to turn for answers. Here is some basic information about the disease.
What is the pancreas?
The pancreas is a glandular organ that sits deep in the abdominal cavity, nestled underneath the liver and adjacent to the first part of the small intestine. The pancreas has several key functions: it secretes insulin, which is critical in controlling blood sugar, and it secretes enzymes into the digestive tract that help break down the fats that we eat so that they can be absorbed.
What is pancreatic cancer?
Pancreatic cancer, or pancreatic adenocarcinoma, is a disease in which specific cells within the pancreas begin to divide inappropriately. This can happen as a result of chronic damage to the pancreas, caused by conditions including chronic pancreatitis. It can also occur if a person has an inherited problem, including specific genetic mutations. However, for the majority of people who have pancreatic cancer, no specific underlying cause is found.
What is the difference between neuroendocrine pancreatic cancer and adenocarcinoma?
Although there are two types of pancreatic cancer, almost everything you hear or read about the disease actually discusses pancreatic adenocarcinoma. This is because adenocarcinoma is overwhelmingly more common than the neuroendocrine form of pancreatic cancer.
Neuroendocrine pancreas cancers make up less than five percent of all pancreatic tumors and are formed by a different cell type within the pancreas, namely the islet cells. Neuroendocrine pancreatic cancers behave and are treated differently than pancreatic adenocarcinoma. Other than their location, the two illnesses have little in common from both a treatment and prognosis standpoint.
What are the stages of pancreatic cancer?
The simplest way to think of pancreatic cancer is in three separate stages:
- Operable disease: the tumor is able to be surgically removed
- Borderline resectable or locally advanced: the tumor is not able to be removed at the moment. Chemotherapy and/or radiation therapy may be able to shrink the tumor and make surgery possible
- Metastatic: the tumor has spread beyond the pancreas and is no longer operable. This is referred to as stage IV disease.
For more detailed information, visit our Stages of Pancreatic Cancer page.
What are the signs and symptoms of pancreatic cancer?
The symptoms of pancreatic adenocarcinoma can be vague and non-specific. These can include abdominal pain with or without back pain, weight loss, bloating, poor appetite, and fatigue. Some people may develop new onset or worsening of diabetes, oily diarrhea (steatorrhea), or yellowing of the eyes or skin (jaundice).
More specific information can be found at our Symptoms of Pancreatic Cancer page.
How is pancreatic cancer diagnosed?
Pancreatic cancer may be suspected when a person goes to the doctor with suspicious symptoms of the disease, such as weight loss, oily stools, persistent abdominal and/or back pain, or jaundice. Typically, a CT scan is done, and a tumor is found on the pancreas. Sometimes tumors in other areas (metastases) are seen as well. There are other tests that may be done to confirm the diagnosis and rule out other conditions. These include an endoscopic retrograde cholangiopancreatography (ERCP), which looks at the pancreatic and bile ducts, and an esophagogastroduodenoscopy (EGD), which examines the stomach, esophagus, and upper part of the small intestine.
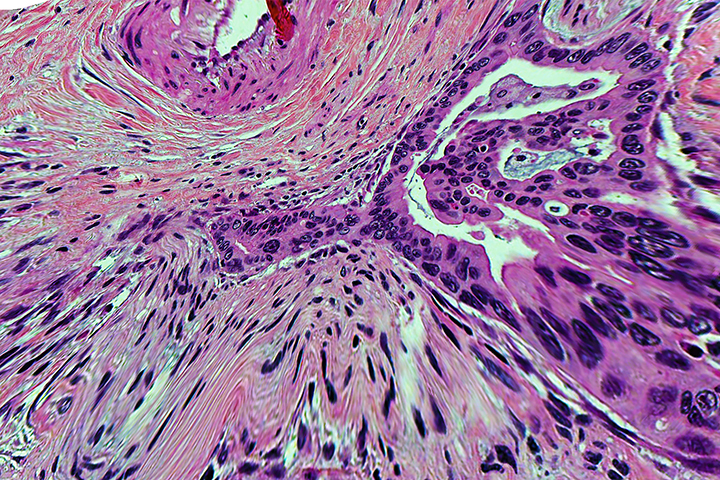
The diagnosis is officially made when a piece of the tumor is taken in a biopsy and examined under a microscope. Adenocarcinoma cancer cells are seen, and the diagnosis of pancreatic cancer is confirmed.
Why is pancreatic cancer often not discovered until it is in advanced stages?
The symptoms of pancreatic cancer are often entirely absent or vague until the disease has spread to other organs, such as the liver. Because the pancreas is located next to the stomach and liver, the abdominal pain that can be associated with pancreatic cancer mimics other, non-cancerous disorders such as reflux, gallbladder problems, or peptic ulcers. Poor appetite, diarrhea, and weight loss can be caused by a large variety of problems. This makes an early diagnosis difficult.
Why is pancreatic cancer so hard to treat?
Pancreatic cancer is difficult to treat for several reasons. In many cases, the cancer is diagnosed in late stages, meaning that the disease can no longer be cured because it has spread to other parts of the body. The cancer may be affecting the patient’s health in ways that make it more difficult to treat. In addition, a thick tissue called the stroma that surrounds the cancer may prevent chemotherapy and activated immune cells from penetrating into the tumor.
Why are clinical trials particularly important for pancreatic cancer?
Although there are treatments available for pancreatic adenocarcinoma, most are not effective in the long term. Because of this, there is a great effort to improve upon current standards. Building upon strong laboratory science and testing new medications or combinations of treatment in clinical trials is the way to best serve current and future patients. Patients who participate in clinical trials may get a treatment that works particularly well for them.
Who is at risk for pancreatic cancer?
There are two types of risk factors for pancreatic cancer: those that can be modified and those that cannot. According to the American Cancer Society, modifiable risk factors include smoking, obesity, and certain chemical exposures. Non-modifiable risk factors include age (the risk of pancreatic cancer goes up as people become older), certain types of pancreatic cysts and genetic risk factors. Finally, chronic ailments such as diabetes, pancreatitis, and cirrhosis of the liver may increase lifetime risk of pancreatic cancer. Non-modifiable risk factors include genetic mutations and inherited syndromes. It is estimated that up to 10 percent of pancreatic cancers are due to a genetic risk factor.
Which genetic mutations and syndromes can make you at higher risk for getting pancreatic cancer?
Mutations in the genes BRCA1, BRCA2, PALB2, STK11, CDKN2A and others are known to increase risk for developing the disease. Families in which certain syndromes are prevalent are also at risk for pancreatic cancer. These syndromes include familial atypical multiple mole melanoma syndrome (FAMMM), Lynch syndrome (also known as hereditary non-polyposis colorectal cancer syndrome), and the Peutz-Jeghers syndrome.
Kim A. Reiss, M.D., is an oncologist at the Abramson Cancer Center, at the Hospital of the University of Pennsylvania in Philadelphia.