Predicting Effective Therapy in Pancreatic Cancer
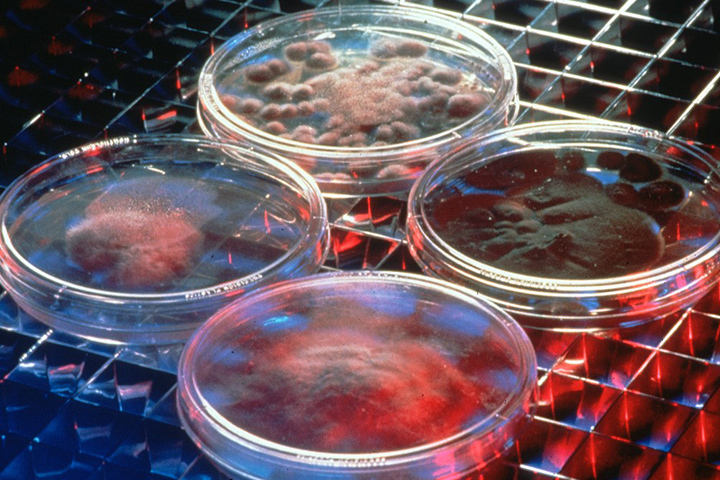
Courtesy of Pacific Northwest National Laboratory
When patients are diagnosed with pancreatic cancer, the first chemotherapy treatment is vital to their survival. But which drug will be most effective?
Editor’s note: After this article was written, Dr. Mark Ricigliano lost his own battle with cancer.
A new clinical trial is exploring how to predict which drug will be successful by personalizing treatment based on a patient’s blood and tissue. Led by Dr. Kenneth Yu, pancreatic cancer oncologist at Memorial Sloan Kettering Cancer Center in New York, and Dr. Mark Ricigliano, a pancreatic cancer researcher and founder/director of Adera BioOncology, the trial is part of Ricigliano’s lifelong work to personalize chemotherapy treatments for pancreatic cancer patients.
“One thing we know is that the better the patient does in the front line, the better the patient’s overall survival and progression-free survival,” says Ricigliano. “So it’s extremely important the patient get the most effective drug early on.”
Choosing Between Two Treatments
In this trial, patients will randomly be assigned to receive one of two first-line chemotherapy treatments for advanced pancreatic cancer: FOLFIRINOX or gemcitabine and nab-paclitaxel. The primary objective is to determine which patients are sensitive to which drugs—meaning they’re more likely to respond better.
For example, a patient who is sensitive to FOLFIRINOX and receives that drug in the trial should do better in progression-free survival (tumor shrinkage, no new metastases, etc.) and overall survival, Ricigliano explained.
The goal is to study these exceptional responders and examine their pharmacogenomic profiles—indicators in the patients’ blood or tissue that can help predict which drugs they’ll respond to. For example, is a specific gene elevated? The hope is that in the future, perhaps a simple blood draw can help doctors determine which drug will work best.
Patients who don’t respond to the drug they’re first given will have the opportunity to get the other drug. If their disease progresses, their full chemosensitivity profile will be given to their treating oncologist, “so there’s a clear clinical benefit to the patient for being in this trial,” explains Ricigliano.
An Organoid for Every Patient
For several years, the Lustgarten Foundation Pancreatic Cancer Research Laboratory at Cold Spring Harbor Laboratory (CSHL), New York, has been developing a technique in which tissue from a patient’s tumor is grown into an organoid. “They’re like little tiny organs,” says Ricigliano, describing the organoids, which are three-dimensional replicas of tumors grown in petri dishes. The hope is that organoids are a better match to the patient’s tumor and can eventually replace growing tumors in mice.
As part of this trial, Ricigliano and Yu are attempting what would be a huge milestone for organoids. Rather than creating organoids from tissue—which requires a biopsy or fine needle aspirate—they’ll try to use a mere blood sample. Not only would this procedure be less invasive for patients, but it would help create organoids faster so that doctors could test drug options for patients in real time.
Ultimately, it’s possible that every pancreatic cancer patient could get his/her own organoid, whether from tissue or blood. This would give doctors a “surrogate model” for each patient’s tumor, explains Herve Tiriac, Ph.D., a research investigator at CSHL. “Our work is to try to determine if it’s a valid idea. We think it is, but we need to prove it.”
Open for Enrollment
Dr. Yu is actively recruiting pancreatic cancer patients to join this trial, which currently has 11 patients enrolled with room for 80 total. Learn more at ClinicalTrials.gov.
Remembering Dr. Mark Ricigliano
Dr. Mark Ricigliano lost his own battle with cancer on May 14. We are deeply saddened, because this is a loss not only for his family, but for the pancreatic cancer community to which he devoted his career. We are moved that his family has asked that donations in his memory be made to Let’s Win, and we send our condolences to those whose lives he touched.






