New Guidelines on the Use of Radiation for Pancreatic Cancer Treatment
How best to use radiation to treat pancreatic cancer patients has been the subject of some intense debate.
But new clinical guidelines from the American Society for Radiation Oncology (ASTRO) may help provide some clarity as to radiation’s use in several different settings.
“Historically, very high rates of distant metastatic disease with pancreas cancer have overshadowed its tendency to recur locally. In the past several years, newer systemic therapies are proving to be more effective at controlling this cancer when it spreads, and fewer people are dying from distant disease. This makes treatments like radiation to manage local disease more meaningful,” said Manisha Palta, M.D., in a prepared statement. Palta served as co-chair of the guideline task force and is a radiation oncologist at Duke Health (Durham, North Carolina). The guidelines also emphasize a patient-centered approach that integrates patients’ values and preferences into treatment decisions, and also stresses the importance of multidisciplinary consultations, planning, and follow-up.
The guidelines present indications for radiation therapy in the adjuvant, neoadjuvant, and definitive settings and delineates between conventionally fractionated and stereotactic radiation therapy, providing the first clinical guidance on the newer, shorter-course approach. “One thing this guideline offers that hasn’t been available previously is context about the current status of ablative radiotherapy such as stereotactic body radiation therapy (SBRT) and where it might be useful for patients with pancreatic cancer,” said Palta.
The guidelines also comment on emerging and upcoming trial reports that will add to the evidence on stereotactic radiation and other aspects of pancreatic cancer treatment, which will shape future clinical practice and guideline updates.
“Any patient who is diagnosed with pancreatic cancer deserves to have a multidisciplinary evaluation, where she or he can have nuanced conversations about the benefits and risks of different types of treatment based on the most current information available. It’s also essential that any patient who might be an appropriate candidate for radiation have access to a radiation oncologist who can provide perspective on the pros and cons of treatment, so that the patient can make an informed decision,” explained Palta. “This is a rapidly evolving field and some potentially practice-changing studies that are not included in this guideline may become available in the relatively near-term future.”
Recommendations for Radiation Treatment
The guidelines were based on a systematic literature review of 179 articles published from May 2007 through January 2017 and developed in collaboration with the American Society of Clinical Oncology (ASCO) and the Society of Surgical Oncology (SSO), which provided representatives and peer reviewers. These guidelines should not be construed as strict or superseding the appropriately informed and considered judgments of individual physicians and patients. The full recommendations can be found at Practical Radiation Oncology.
- In the adjuvant/postoperative setting, conventionally fractionated radiation is recommended conditionally for patients with high-risk features such as positive lymph nodes and margins following surgical resection. SBRT is recommended only if the patient is enrolled in a clinical trial/data registry.
- In the neoadjuvant/preoperative setting, conventionally fractionated radiation therapy or SBRT is recommended conditionally following chemotherapy for patients with resectable disease. Neoadjuvant chemotherapy plus radiation (either conventional or stereotactic) is conditionally recommended following systemic therapy for select patients with borderline resectable disease.
- For patients with locally advanced disease (who are not candidates for surgery), systemic chemotherapy followed by either chemoradiation or SBRT is recommended conditionally as an option for definitive treatment.
Recommendations also address optimal dosing for various subgroups of patients, sequencing of radiation with systemic chemotherapies, simulation and setup strategies, techniques for treatment planning and delivery, and treatment in the palliative setting.
Ongoing Studies for Pancreatic Cancer Treatment
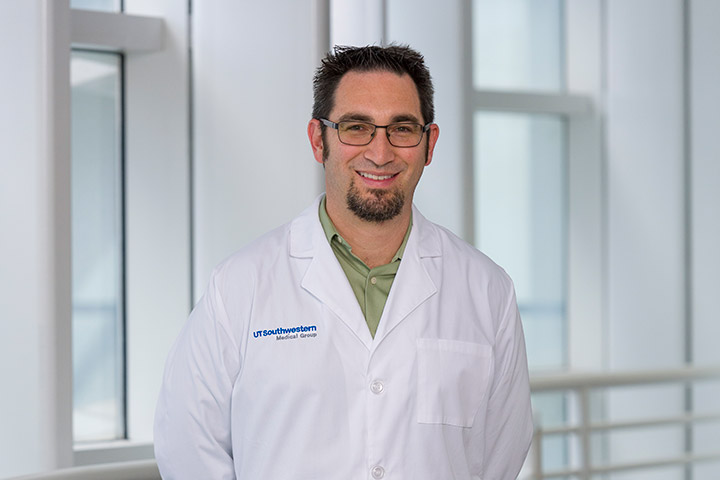
The role of radiation in pancreatic cancer has been controversial for “a couple of decades,” says radiation oncologist Dr. Theodore Hong, Professor, Radiation Oncology, Harvard Medical School and Director, Gastrointestinal Service, Radiation Oncology, Massachusetts General Hospital (MGH), Boston.
“Conventional doses of radiation are unlikely to impact long-term survival, as the doses are not ablative and are unlikely to produce complete responses,” he adds. “But these modest doses of radiation may improve resectability and subsequently survival in the borderline resectable setting, as demonstrated in the PREOPANC and Korean randomized trials. If the goal is to ablate an unresectable tumor, then higher doses of radiation must be used, as demonstrated in series [collection of information on more than one patient] with MRI-delivered therapy, high dose external beam radiation as demonstrated by Dr. Chris Crane [at Memorial Sloan Kettering Cancer Center (New York)], or adding a boost with intraoperative radiation therapy, as per MGH,” Hong says. He notes, “It is important not to consider all radiation equivalent.”
In the resectable setting, a trial comparing chemotherapy regimens with or without radiation will answer whether postoperative radiation improves outcome, albeit with non-FOLFIRINOX based chemotherapy, Hong says. And due to better chemotherapy regimens, there will need to be clarity for the role of neoadjuvant radiation in the setting of a total neoadjuvant approach in both the resectable and borderline settings. One trial that may provide some answers randomized patients between preoperative FOLFIRINOX and FOLFIRINOX followed by hypofractionated radiation therapy for borderline resectable pancreatic cancer. Although this is a very straightforward study, there are concerns regarding the learning curve needed to comfortably explore patients after this regimen due to the fibrosis associated with this radiation regimen, Hong says, adding the optimal preoperative radiation schedule and fields remains unknown.
Regarding unresectable disease, Hong believes that a demonstration of feasibility of ablative doses of radiation to pancreatic cancers beyond a few select institutions needs to be demonstrated before this approach can be tested in a randomized trial. “However, this is one of the more exciting areas in radiation and pancreatic cancer and represents an interesting intersection between technology and patient outcomes,” he says.
Escalated radiation therapy with MRI-guided delivery and adaptive planning as well as other ways to boost dose like intraoperative radiation are exciting and are currently being analyzed in the setting of multicenter clinical trials, Hong says. There are also drug/radiation combinations that hold exciting promise for systemic efficacy, he says.
In an abstract at ASCO GI 2019, Dr. Aparna Parikh (MGH) and colleagues demonstrated systemic response to immune therapy was possible in patients with MSS pancreatic cancer when adding radiation to ipilimumab and nivolumab. This approach has been integrated into a multi-institutional randomized trial sponsored by the Pancreatic Cancer Collective, a Lustgarten Foundation/Stand Up To Cancer collaboration.