Machine-Learning Assay May Improve Pancreatic Cyst Management
Pancreatic cysts are all too common, and the numbers seem to be growing.
One of the culprits in this increasing incidence is the sheer numbers of people who undergo abdominal imaging for a variety of ills. Pancreatic cysts are then being found incidentally. Although most cysts cause few, if any, symptoms and won’t progress to cancer, some will, especially two types of mucin-producing cysts, called intraductal papillary mucinous neoplasms (IPMNs) or mucin-producing neoplasms (MCNs). Methods for figuring out what type of cyst a patient has and which of these mucin-producing cysts may be headed toward malignancy are imperfect. This results in extensive monitoring, imaging, and too often, complicated and unnecessary surgeries.
A new assay called CompCyst, developed by researchers at Johns Hopkins’ Sidney Kimmel Comprehensive Cancer Center (Baltimore, Maryland), could potentially change how doctors manage these cysts, according to a study published in the journal Science Translational Medicine. CompCyst is based on a branch of artificial intelligence called machine learning, which essentially teaches a computer to “learn” for itself and improve with experience.
In this proof-of-concept study, the Johns Hopkins researchers, who led an international scientific team, tested millions of combinations of features to identify markers that predict the best treatment pathway for an individual cyst. The test showed high degrees of sensitivity and specificity, which means that CompCyst appears to be able to correctly identify those cysts that are very likely to turn into cancer as well as those that will remain benign.
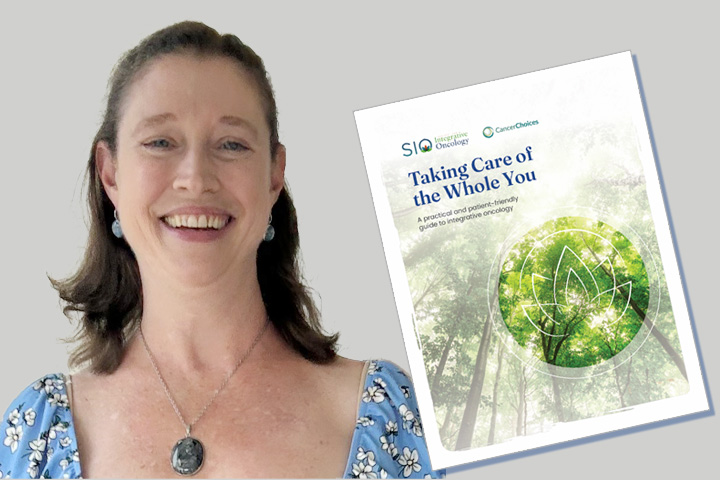
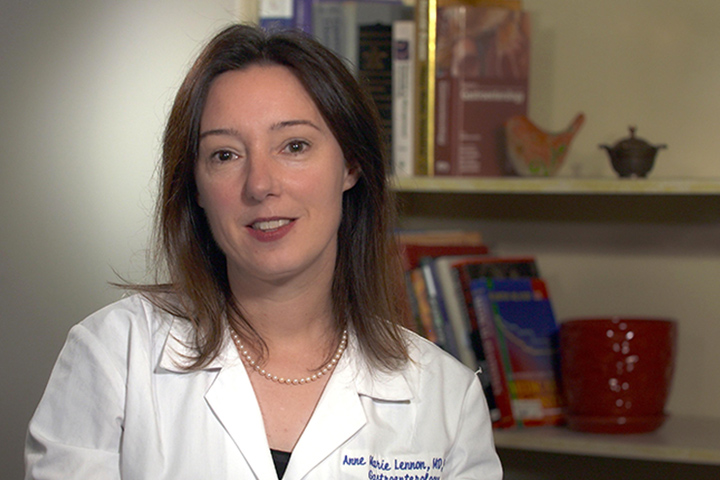
“I can honestly say that I am very excited about this,” explains Dr. Anne Marie Lennon, assistant professor of medicine and director of the Johns Hopkins Multidisciplinary Pancreatic Cyst Clinic. “Our goal would be to be able to tell a patient you have a cyst which has no risk of turning into cancer, go home, don’t worry,” she says. “But right now we can’t do that because the tests we have currently are not sufficiently accurate to determine this.”
With pancreatic cancer among the most deadly of diseases, finding an accurate method that could tell doctors that immediate surgery is necessary, or that patients need to be monitored for a period of time—generally several years—or that they can go home and don’t need to come back, could potentially revolutionize cyst management, she adds.
A Pancreatic Cyst Evaluation Primer
There are several types of pancreatic cysts, and some present a real clinical challenge. Benign pancreatic pseudocysts aren’t new growths or even cysts, but rather are comprised of fluid that leaks out of the pancreas after an injury or as a result of a bout of pancreatitis. Serous cystadenomas (SCAs) are true cysts, but carry no risk of becoming malignant. But doctors may do biopsies and endoscopic ultrasounds to figure out of if the cyst is actually an SCA.
Among the most worrying of cysts are mucinous cystic neoplasms (MCNs) and intraductal papillary mucinous neoplasms (IPMNs), which are both mucin-producing. Mucin is a glycoprotein component of the mucous that coats the surfaces of cells lining body systems like the respiratory and digestive tracts. MCNs are precancerous and can sometimes be confused with pseudocysts, and may require surgery, or follow-up per established guidelines. IPMNs are the most common type of cyst and need to be evaluated and monitored regularly to make sure they don’t become malignant.
“The reason we’re interested in pancreatic cysts is because two types of the three precursors to pancreatic cancer are the IPMNs and MCNs,” says Lennon. She adds that they are easily identified with CT and MRI and offer the opportunity to potentially screen for pancreatic cancer. Current consensus guidelines recommend that patients with mucin-producing cysts undergo surveillance, and those mucin- producing cysts which harbor either cancer, or are at the stage just before cancer, called high-grade dysplasia, should undergo surgical resection. Patients with a mucin-producing cyst without high-grade dysplasia or cancer should undergo surveillance, Lennon says. Occasionally, pancreatic ductal adenocarcinomas, what we know as the most common form of pancreas cancer, or neuroendocrine tumors can present as a cyst.
“From a clinical perspective the key decisions we need to make are: does the patient have a type of pancreatic cyst that has minimal or no risk of developing cancer and can be discharged, or do they have a cyst with cancer or high-grade dysplasia that requires surgical resection, or do they have a mucin-producing cyst which can be followed,” Lennon explains. “We always err on the side of caution.”
Erring on the side of caution is the real issue, since the majority of these cysts will never become malignant. “There are so many patients with cysts and virtually all need to be followed since we can’t really accurately differentiate what type of cyst a patient has,” Lennon says. “If no surgery is performed, we might miss a cancer. But a patient might also undergo surgery who truly doesn’t need it, and the surgery itself is tough and has the potential for some complications that can really affect quality of life.”
Enter CompCyst
The researchers analyzed a cohort of 862 pancreatic cyst patients, all of whom had undergone surgical resection. Molecular, clinical, and imaging data from 436 of these patients was used in the machine-learning algorithm to classify these patients into three cysts categories: those that had no risk of cancer and could be discharged; those that harbored cancer, or high-grade dysplasia and needed surgical resection; those with mucin-producing cysts (IPMNs and MCNs) with no cancer or high-grade dysplasia who could be safely watched. The CompCyst test was then compared with current clinical practice in the remaining 426 patients, which formed a validation cohort.
According to trial results, CompCyst outperformed current clinical practice in identifying all three patient groups. Current clinical management correctly identified only 19 percent of patients with a benign cyst who could be discharged, whereas the CompCyst test correctly identified 60 percent of them. For cysts that should be monitored—mucin-producing cysts without high-grade dysplasia or invasive cancer—current clinical management correctly identified 34 percent of these, whereas CompCyst correctly identified 49 percent. CompCyst and current clinical management both performed well in identifying patients with cysts which required surgery, identifying 91 percent and 89 percent of patients respectively. Overall, the authors calculated that the use of CompCyst could have avoided unnecessary surgery in 60 percent of the patients included in the study.
What’s Next
The hope is to make CompCyst available to Johns Hopkins pancreatic cyst patients within the next nine to 12 months. From there, they plan to launch a prospective study of about 1,000 patients. The ultimate goal, of course, would be to add CompCyst to the resources doctors currently use in pancreatic cyst management.
The current study did have some limitations, including the fact that the types of cysts being analyzed were not those routinely found in clinical practice. “There are more questions to be answered and we need to do a prospective study, but as a clinician I know we need better tools to help our patients,” Lennon says. “What’s exciting is that we are adding to current knowledge through very sophisticated molecular analysis, without disregarding the tools we have now.”