Finding the Best Diabetes Drug for Pancreatic Cancer Patients

While diabetes is a risk factor for the development of pancreatic cancer, cancer and its treatments can also cause hyperglycemia (elevated blood sugar), creating another set of issues for patients.
Chemotherapy, the backbone of advanced cancer treatment, comes with a host of well-known side effects, including potentially an increase in blood sugar. Pancreatic cancer itself can cause hyperglycemia through processes that are still not fully understood. Doctors generally choose between two different classes of medications to help control blood sugar in these patients. Yet, there is little evidence to support choosing one class over another.
The Need for Evidence-Based Treatment
Endocrinologist James Flory, M.D., of Memorial Sloan Kettering Cancer Center (New York City) wants to change that.
Flory, an expert in the treatment of cancer patients with hyperglycemia, is proposing a new study to compare the effectiveness of diabetes drugs in supportive care for pancreatic cancer patients. “There unfortunately isn’t much research in this area, and we need evidence in order to choose the best drugs for this patient population, especially in terms of improving their quality of life,” he says. “For example, some anti-diabetes drugs promote weight loss and that’s great for a diabetic patient without pancreatic cancer. But it’s certainly not that great for a pancreatic cancer patient.”
The causal link of pancreatic cancer to diabetes has been well established. Although about 50 percent of pancreatic cancer patients have diabetes at the time of diagnosis, about 80 percent will develop hyperglycemia while being treated. More than 30 percent will receive treatment with antidiabetic drugs, generally metformin or a class of older drugs called sulfonylureas.
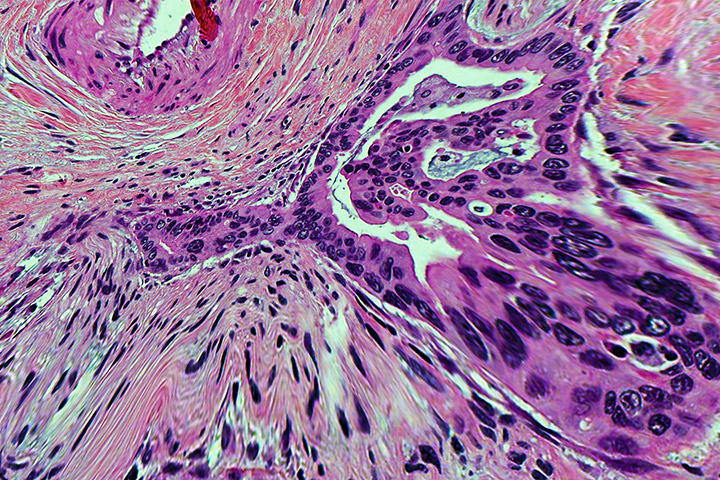
Metformin is in a class of medication called a biguanide. With metformin, blood glucose levels are primarily lowered by decreasing the amount of glucose produced by the liver, and by making muscle tissue more sensitive to insulin so glucose can be absorbed. Most experts consider metformin to be the safest medicine for type 2 diabetes because it has been used for many decades and is effective, affordable, and has few side effects. Metformin is recommended as a first-line treatment for type 2 diabetes by the American Diabetes Association. Sulfonylureas, which first came to prominence in the 1950s, work differently. These drugs stimulate the beta cells of the pancreas to release more insulin.
The side effects of metformin can include nausea, vomiting, diarrhea, stomach upset, a metallic taste in mouth, and loss of appetite. Perhaps because of these side effects, metformin seems to cause a little weight loss. On the other hand, sulfonylureas may cause blood sugar to go too low, but they can also cause hunger and weight gain.
Flory is especially concerned about the weight loss component of metformin. That’s because about 85 percent of patients with pancreatic cancer develop cachexia, which is associated with weight loss, muscle loss, a lack of appetite, fatigue, and decreased strength. About 30 percent of pancreatic cancer patients die from problems associated with cachexia, rather than the degree of tumor burden associated with their illness.
“I need to be clear, metformin is a great drug, a very safe drug,” Flory notes. “And the choice between using metformin in this population rather than a sulfonylurea often comes down to clinical preference. We need more evidence on what may be best for patients not only in terms of managing blood sugar, but also their quality of life, which is an important aspect of care.”
The Proposed Study
The study design is that of a “pragmatic” research trial, Flory explains. A double-blinded clinical trial is a type of trial most often falling into the realm of an “explanatory” trial, he adds. Explanatory trials evaluate the effect of treatments in ideal conditions, while pragmatic trials evaluate the effect of treatments in routine, everyday practice.
The researchers hope to enroll 132 patients with hyperglycemia and pancreatic cancer in a pragmatic randomized trial comparing metformin to sulfonylurea. Weight change will be the primary outcome. Quality of life as measured by an established questionnaire specific to quality of life in pancreatic cancer will also be included as a secondary outcome. Severe hypoglycemia will be a key safety outcome.
“We really hope to get this off the ground,” Flory says. “I meet with cancer patients all day. We have an incredible pancreatic cancer team at Sloan Kettering, and I’m really thrilled to be joining with them on this proposed study. Pancreatic cancer is one of the toughest cancers to treat and the disease can be very hard on people.
“Cachexia is difficult for patients, and it can be tough for their caregivers too, the people who love them. So if we focus on a common choice in supportive care between two effective drugs like metformin and sulfonylurea we can get to some answers that can improve clinical practice and really enhance the quality of life for these patients. Quality of life can’t be ignored. It’s an important aspect of care. And gaining some weight could make a world of difference for some patients in terms of their quality of life.”