Living Longer with Pancreatic Neuroendocrine Tumors

They are words you don’t often hear together: “Metastatic cancer” and “hope.”
But that’s exactly what Dr. Pamela Joy Hodul offers her pancreatic neuroendocrine tumor (PNET) patients; hope, if not for a cure, then for prolonged survival and a good quality of life. “Even in the metastatic setting, there are many treatment options. It is possible to keep setting the clock back on the progression of the disease,” says Hodul, surgical oncologist at Moffitt Cancer Center in Tampa, Florida, and Associate Professor in the Division of Oncologic Sciences at the University of South Florida.
PNETs are not your average pancreatic tumors. Recently thrust into the spotlight again with the death of soul legend Aretha Franklin, and Apple founder Steve Jobs before that, both of whom died from pancreatic neuroendocrine tumors, PNETs are quite rare. They account for about 6 percent of all pancreatic cancers.
They differ from the more common adenocarcinomas in many ways. They tend to grow much more slowly. They strike nearly two decades earlier (around age 40, as opposed to age 60). Their prognosis is a bit better. There are several subtypes, some of which are benign. And there tend to be more treatment options. There is a chance for a complete cure if caught early. Most PNETs are discovered incidentally during an exam for other conditions or unrelated symptoms.
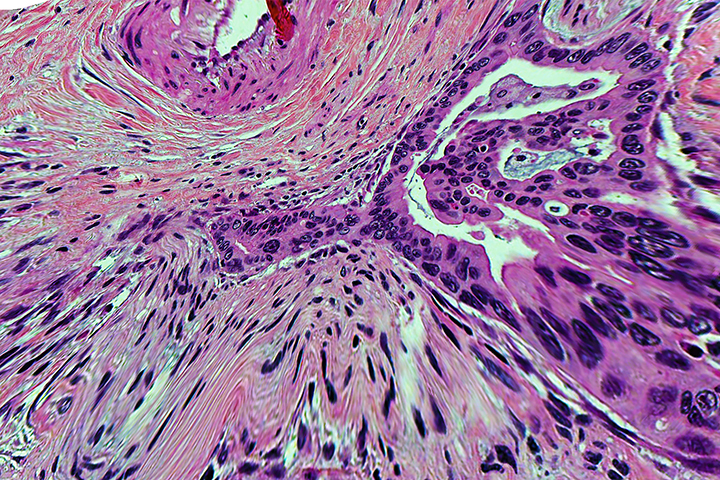
Indicative Islets
As the name suggests, neuroendocrine tumors are linked to the endocrine system. They develop from the abnormal growth of endocrine (hormone-producing) cells in the pancreas called islet cells.
Neuroendocrine tumors also occur in other parts of the gastrointestinal system and elsewhere in the body. Even within the pancreas, there are different types of NETs, depending on which islet cells are involved. Some cells produce insulin (which lowers blood sugar levels) or glucagon (which raises blood sugar levels). Others produce somatostatin, which regulates the levels of a variety of other hormones in the blood, or gastrin, which stimulates secretion of gastric acid.
PNETs can also be either functional (produce hormones) or nonfunctional (produce no hormones). Functional neuroendocrine tumors are usually easier to spot because they cause the pancreas to overproduce hormones, resulting in hormone-related symptoms. Someone with a functional insulinoma, for instance, would have extra insulin in their system and may start overeating in order to squash feelings of hunger and shakiness. Someone with a gastrinoma would have extra gastric acid in their system, causing reflux, abdominal pain, or ulcers.
Most PNETs are nonfunctional, however, and may not be detected until the tumors have progressed to a later stage, or spread to other organs. “Unless they are secreting excess hormones, the tumors could be there for years before they are found,” Hodul explains.
The ideal way to diagnose a PNET is by endoscopic ultrasound, in which a biopsy can also be taken in a way which decreases the risk of “seeding” (the unintentional release of some tumor cells as biopsy needles are pulled out of tumors, which can result in spreading the cancer) into surrounding tissues. But PNETs can also be identified by distinctive proteins that stand out on stained pathology slides.
Blood tests are helpful as well in diagnosing functional PNETs, as they can measure some of the telltale hormones and other tumor markers, such as pancreatic polypeptide levels. The tumors are then imaged using PET scans, either with nuclear tags or Hodul’s preferred method, a DOTATOC study, which uses an amino acid peptide bound with radioactive nucleotides, and tags with high affinity to hormonal receptors.
Expanded Options for PNETs
Based on information provided by these tests, doctors are presented with several treatment options, Hodul explains. The surgical principles for PNETs are essentially the same as for adenocarcinomas. Tumors contained within the pancreas and not tied up in any blood vessels may be candidates for surgical removal. Larger tumors, or those in difficult locations, might be able to be shrunk with chemotherapy and operated on later.
Doctors also have additional tools in their kits for neuroendocrine tumors, however. These include injections of medicines that block the hormones feeding the tumors, or of radioactive molecules that bind to peptide receptors and deliver super-targeted therapy.
For those whose tumors have spread to other organs, such as the liver, interventional radiology procedures such as embolization to cut off the tumor’s blood supply, or ablation to burn it away, may be options. Neuroendocrine cancers often respond well to these interventions, and as long as doctors can continue to “debulk” the tumors, the cancer can stay at bay for years, adds Hodul.
Careful Planning
The scope of options and varied aspects of the disease in all its personal permutations means specialist advice should be sought, however, especially when developing an initial treatment plan. Subsequent treatments could then be delivered locally. “Most medical professionals are not familiar with all the treatments, nor the order in which they should be engaged. Many may see only one of these cases per year, or in their lifetime,” Hodul notes.
Luckily, there are several centers specializing in neuroendocrine tumors scattered around the United States, including the Mayo Clinic in Arizona and Minnesota, MD Anderson Cancer Center in Houston, Texas, and the University of California, San Francisco. Hodul works at Moffitt Cancer Center in Florida, one of the highest-volume NET treatment centers, with about 300-400 cases per year. She has also engaged in remote consultations with oncologists across the country, saying “It’s important to reach out to local and national support groups, who can help steer you in the right direction.”
PNET patients should be optimistic as they face the disease, Hodul says. “The disease progression is very different from other types of cancer, and should give hope to PNET patients. Treatment can be very beneficial in most cases, even in metastatic disease.”