Using A Virus to Reach the Tumor

Humans are all too familiar with viruses, the microscopic infectious agents that cause havoc with health.
Unable to do much on its own because of its simple structure, the virus is like a parasite and must infect a host to begin its relentless march of replication. The end results are diseases like the common cold, COVID-19, the flu, and HIV, among so many others.
But what if scientists could harness the power of the virus to beat back cancer? For two cancers, such agents have already been approved, one to treat metastatic melanoma and the other to treat a specific form of bladder cancer. Scientists are hoping to expand the scope.
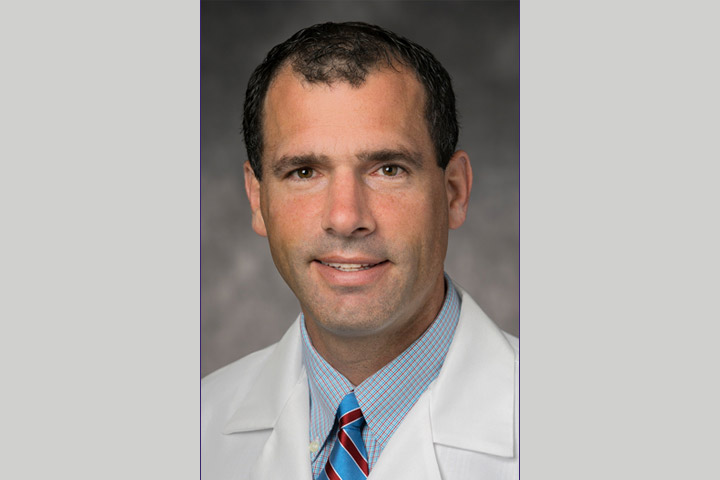
“I had a friend and colleague who was working on the oncolytic virus for melanoma and the more I heard about it, the more I was convinced that maybe there’s something to this approach that could potentially help with other forms of cancer,” says gastrointestinal oncologist Tara Seery, M.D., Director Hepatobiliary Cancer and Co-Director Cell Therapy at the Hoag Family Cancer Institute, Newport Beach, California. Seery is an investigator on a phase IIb trial looking at an oncolytic viral agent called VCN-01 in combination with chemotherapy for the treatment of pancreatic cancer. “The oncolytic virus treatment for some patients with melanoma gave people their lives back,” she explains. “We need to do the same thing for people with pancreatic cancer. Combination therapies are showing some promise so we will have to see how this trial evolves. But I am hopeful about the potential.”
An Oncolytic Virus Primer
The idea of using a virus to treat cancer isn’t exactly new. Scientists have been experimenting with the idea off and on for decades. Oncolytic viruses exploit basic biology. Very simply, healthy cells have the ability to make copies of their genetic information and to reproduce. But once infected by a virus, a cell is forced to make copies of the virus’ genetic material. The process is relentless, often resulting in more viruses and infected cell death. But oncolytic viruses, which are changed so they can’t cause illness, are programmed to specifically target, infect, and kill cancer cells, while leaving healthy cells alone.
About the Study
Pancreatic cancer is particularly difficult to treat in later stages. That is due, in part, to the stroma, a dense, fibrous cocoon surrounding the pancreatic tumor. That barrier shields the cancer, making treatments like chemotherapy and immunotherapy less effective.
According to Theriva Biologics, the developer of VCN-01, this virus is intended to break down the tumor’s protective barrier, the stroma. It is also designed to expose the tumor to robust and persistent attack by the patient’s immune system.
In the VIRAGE phase IIb clinical trial, VCN-01 plus standard-of-care chemotherapy with gemcitabine/nab-paclitaxel is being evaluated as a first-line therapy for patients with metastatic disease. VCN-01 has been granted Orphan Drug Designation and Fast Track Designation by the U.S. Food and Drug Administration (FDA) for the treatment of pancreatic cancer. Fast Track Designation is a process designed to facilitate the development, and expedite the review of, drugs to treat serious conditions, fill an unmet medical need, and get important new drugs to the patient earlier, according to the FDA.
“Rapid progress in the VIRAGE trial is a testament to physician interest in VCN-01 and the significant unmet need for an effective treatment for this deadly disease,” said Steven Shallcross, Chief Executive Officer of Theriva Biologics in a statement. “We are currently planning regulatory engagements to discuss next steps in VCN-01 clinical development, including the potential for an interim data analysis.”
The VIRAGE trial is being conducted at numerous sites across the U.S. and Europe. The target enrollment of 92 evaluable patients has been met. In both the control and treatment arms, patients are treated with gemcitabine/nab-paclitaxel standard-of-care chemotherapy in 28-day cycles. In the treatment arm only, patients also receive single doses of intravenous VCN-01, administered seven days prior to the first and fourth cycles of gemcitabine/nab-paclitaxel treatment. Primary endpoints for the trial are overall survival and VCN-01 safety and tolerability. Additional endpoints include progression-free survival, objective response rate, and measures of biodistribution, VCN-01 replication, and immune response.
“What drove me to the trial is how this virus interacts with the stroma,” says Seery. “If drugs can be designed and combinations can be designed to penetrate or destroy the stroma, we can treat patients more effectively. Patients with metastatic pancreatic cancer need more options that are tolerable and effective. We need to do better than just chemotherapy.”