Testing Vitamin C as a Cancer Killer
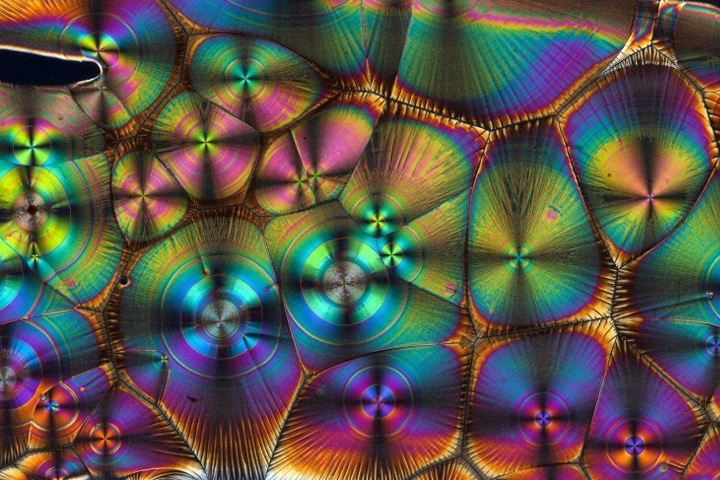
Kevin MacKenzie, University of Aberdeen; Wellcome Images
In April 2016, Let’s Win reported on a study that found that in the lab, vitamin C was effective against colorectal cancer cells with KRAS and BRAF mutations.
These same mutations are found in over 90 percent of pancreatic cancer cases.
The concentration of vitamin C needed to make a therapeutic difference—10 grams, or the equivalent of the vitamin C found in 300 oranges—cannot be achieved orally, so standard vitamin supplements would not be effective. Now scientists are moving rapidly to identify what might work for human cancer patients, and how to administer it.
Clinical Trials for Vitamin C
It usually takes about 15 years for lab discoveries to find their way into clinical use, but scientists at the Meyer Cancer Center of Weill Cornell Medicine in New York City—led by Lewis Cantley, Ph.D. (now at Harvard Medical School, Boston)—are on track to make it happen in 15 months.
With the support of private donors and the Lustgarten Foundation, they have just launched human trials to validate their initial lab-based findings and ensure the doses can be safely administered intravenously. Vitamin C has a very good safety profile, with low toxicity, so the scientists and clinicians are optimistic about the first stage trial.
As part of a $12 million award from Stand UpTo Cancer, the researchers will be able to conduct additional trials on two cohorts of patients, allowing them to identify who is most likely to respond, learn more about the basic science mechanisms involved in the responses, and collect some early evidence of clinical benefit.
The first group of patients will be those about to undergo surgery for colon, pancreatic, or lung cancer. In the four weeks leading up to their surgery, they will receive regular two-hour vitamin C infusions, up to four days per week.
Scans will be taken at the beginning and end of that period, and samples of their tumors collected during their surgery. Those samples will undergo extensive genetic sequencing, and pieces of the tumors will be grown as “organoids” that could be further studied and transplanted into mice.
Researchers won’t know the patients’ mutation statuses until after the trial is already underway, but that information will be used afterwards to see how patients with KRAS and BRAF mutations responded compared to those without those mutations.
“We would expect and hope to see some tumor shrinkage among those with KRAS and BRAF mutations,” Cantley says. “Increased time to progression or quantified stable disease would also be considered a good response.”
The second group will be previously treated patients known to have KRAS or BRAF mutations, whose tumors were non-responsive to traditional therapies, or whose diseases had metastasized. They will receive the same infusions, for up to six months, with a three-month check to see disease response.
If there appears to be a clinical benefit that suggests further investigation is warranted, additional trials could be designed to determine optimal efficacy and dosage, and to compare therapeutic results against other treatments, such as current chemotherapy-based standard of care or combination therapy.
How Vitamin C Fights Cancer
The conventional wisdom is that vitamin C improves health in part because it can act as an antioxidant, preventing or delaying some types of cell damage. However, Cantley and his colleagues discovered that the opposite was true in regards to high-dose vitamin C’s therapeutic effects for the KRAS and BRAF forms of colorectal cancer: they occur as a result of inducing oxidation in these cancer cells.
Cancer cells whose growth is driven by a mutation in the genes KRAS or BRAF make unusually large amounts of a protein that transports glucose across the cell membrane. The transporter, GLUT1, supplies the cells with the high levels of glucose they need to survive. They also produce a large amount of reactive oxygen species (ROS). As it turns out, this combination of events creates the perfect storm for these tumors to be killed by vitamin C. The high ROS converts the vitamin C (ascorbate) that is flowing in the blood stream outside the cancer cells into dehydroascorbic acid (DHA). GLUT1 not only lets glucose into cells but also transports the DHA into the cell.
Cantley’s team found that once inside, the DHA acts like a Trojan horse. Natural antioxidants inside the cancer cell attempt to convert the DHA back to ascorbic acid (vitamin C); in the process, these antioxidants are depleted and the cell dies from oxidative stress.
“While many normal cells also express GLUT1, KRAS-mutant and BRAF-mutant cancer cells typically have much higher levels since they require a high rate of glucose uptake in order to survive and grow,” Cantley notes. “Also, KRAS and BRAF mutant cells produce more reactive oxygen species than normal cells and therefore need more antioxidants in order to survive. This combination of characteristics makes these cancer cells far more vulnerable to DHA than normal cells or other types of cancer cells.”
Initial lab tests showed that exposure to large doses of vitamin C killed cultured cells with BRAF or KRAS mutations, and daily high dose injections to mice engineered to develop KRAS-driven colon tumors caused the mice to develop fewer and smaller colon tumors compared with control mice.
Cantley is excited about applying the results to humans and expanding the trial to include other cancer types. “The impact of high-dose ascorbate across malignancies should be highly informative, since different tissues have different metabolic states,” he adds.