A Second Opinion Saved My Life!

- Severe abdominal pain starts my cancer journey
- Difficult recovery after Whipple procedure
- Living with chronic nausea
My name is Janet McNabb and I am a pancreatic cancer survivor.
My cancer was diagnosed in September 1996, although I am sure much has changed since then. I had been having so much pain in my abdomen and a lot of indigestion. I first noticed the pain when riding in the car on long trips.
I was working as a registered nurse in the OR at the time. I went to my local gastroenterologist, in Myrtle Beach, South Carolina, where I live. My doctor first did an EGD (a test to examine the lining of the esophagus, stomach, and duodenum) and determined that I had stomach bacteria, so he treated me for it.
The pain continued. Often, it got so bad that I had to be helped out of the OR. When this happened I would be taken to same-day surgery, sedated, and someone would have to take me home. This continued for 15 months. My GI doctor suggested having my gallbladder removed, so I did it. Unfortunately, my surgeon said there was nothing wrong with my gallbladder; the surgery hadn’t been necessary at all. He was not happy with my GI doctor.
The pain persisted and I continued to put up with it for several more months. Finally, my doctor came to see me after one of these episodes. He told me there was nothing else he could do and I had to learn to live with the pain.
I Get a Second Opinion
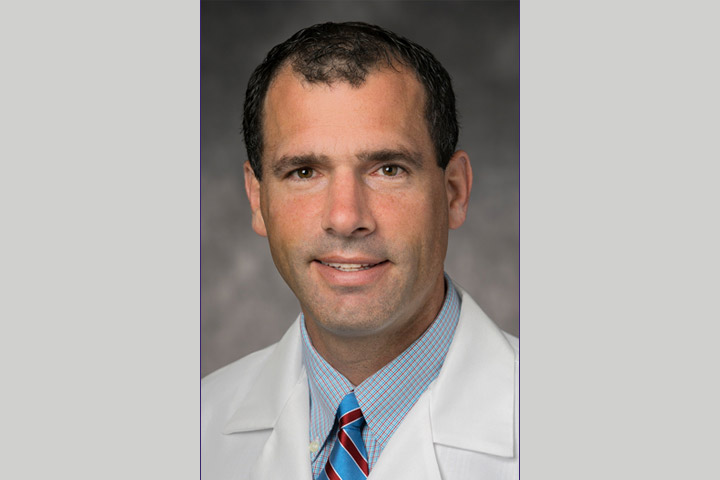
I continued to have severe pain in the middle of my stomach, which also radiated into my back. My husband Bill told me to get another opinion, but I was hesitant. Bill insisted that I ask someone at work who I should see in Charleston at The Medical University of South Carolina (MUSC). My good friend Dr. Fred Bellamy, an anesthesiologist, who had done his residency at MUSC, told me to see Dr. Bill Marsh. I made an appointment with him not knowing he had left MUSC.
I went to see Dr. Marsh with my husband and within 15 minutes he said I needed an endoscopic retrograde cholangiopancreatography (ERCP), which is a procedure that combines upper GI endoscopy and x-rays, used to treat problems of the bile and pancreatic ducts. I received a call from Dr. Paul Tarnasky’s office at MUSC to schedule an ERCP. On August 14, 1996, my husband and I went to Charleston for the procedure. Per insurance, they had to check the bile ducts first. They found the pressures to be extremely high and did a sphincterotomy of the bile duct instead. I went home but within a few days I was so sick I couldn’t sit up. I called Dr. Tarnasky and he said I needed to return for an ERCP of my pancreatic duct. The appointment was scheduled for the following week.
An Experimental Stent Leads to Cancer Diagnosis
Once again, we traveled to Charleston for the ERCP. Before the procedure, Dr. Tarnasky asked if we wanted an experimental stent placed into the duct. He explained it would require me staying overnight and undergoing another ERCP the next morning to remove the stent. He said it seemed to decrease the chances of pancreatitis up to 40 percent. We could have easily said no, but we said OK. This is the only experimental treatment I have ever tried . . . and I am so grateful for it.
The ERCP was performed and a stent was put into place. He took some biopsies at that time. The next morning he performed another ERCP. To his surprise, he found that the stent was gone! It didn’t stay in place and probably passed through my system. But he saw a tumor on the head of the pancreas.
When they told my husband Bill what they found, he asked if he could be the one to tell me. They agreed. He told me, “There’s a little problem, but it’s going to be ok.” I asked, “What is it?” He said, “They found a tumor, but you’re going to be OK.” He never mentioned the word “cancer.” I didn’t believe him at first. He assured me he was telling me the truth. I was stunned. I felt like my fate was sealed. I was a registered nurse and I just knew I probably had three to six months to live.
I would need a colonoscopy and possibly a bowel resection as polyps often go along with this. I also needed to meet with the pancreatic specialist for surgery, Dr. David Adams.
There were a couple of weeks between the procedures. Dr. Tarnasky told my husband to take me home and fatten me up some because I was so little. Plus, they were waiting on the biopsy reports. I told my husband I wanted to go to Virginia, where we were from. I wanted to go hiking, roast hot dogs and marshmallows over an open fire, and go fishing. So we did exactly that with some friends that lived there. We also visited relatives and my best friend Vicky (she died of pancreatic cancer in 2005).
When we returned home, I had an appointment for the colonoscopy with Dr. Tarnasky on Friday, September 6. I was called by Dr. Tarnasky’s office the day before and was told they were closing due to an impending hurricane. Well, I didn’t go in for the colonoscopy and my consult with Dr. Adams that Friday. I received a call from Dr. Adams’ office wanting to know where I was. I told them I had been called and my appointment was canceled by Dr. Tarnasky’s office. We rescheduled both appointments for Monday, September 9 to see Dr. Adams and have the colonoscopy.
A Whipple Procedure on Friday the 13th
When I met with Dr. Adams, he said I had cancer. After the colonoscopy and another ERCP, Dr. Adams came back in to talk to my husband and me. He said the tumor was growing fast and that it was cancerous. He then asked, “Do you want surgery on Wednesday or Friday?” I was shocked and said, “OF THIS WEEK?!” He said, “Yes, the tumor is growing so fast we can’t wait.” I said, “Well, give me a couple of days to prepare.” Friday was the 13th, so I asked if he was superstitious since it would be Friday the 13th. He replied, “Nope, I do my best work on the 13th.”
On Friday, September 13, I had the Whipple procedure. My husband and children were there. (My children were already grown by then.) The surgery went well, but I have to say it was the worst thing I have ever been through. My husband had planned on staying a couple of days but ended up staying 10 full days when he saw how bad it was. I could NEVER have done it without him! He took fantastic care of me and wouldn’t leave my side. He learned a lot of things about how to care for me. The nurses were so busy and couldn’t always come quick enough. I went through a lot and he was there to demand things be done.
I never knew what a horrible experience it was going to be. I was NOT PREPARED! I worked as a registered nurse in surgery and had never done a Whipple procedure nor cared for a Whipple patient. I was taken by complete surprise and expected to be better faster. You have to realize this is the biggest surgery you can have done. IT WAS NOT EASY but they SAVED MY LIFE.
On Thursday after my surgery, Dr. Adams told me they had removed all of the cancer and that there was no need for chemo or other treatments. He also told me that had I waited another two months it would have been too late. Thank God Bill insisted that I go for a second opinion.
My Life After the Whipple Procedure
It took me six months after the Whipple procedure to try to return to work. When I did, I found it impossible to work full-time, so I went part-time. But I had unpredictable nausea and often couldn’t get up to go to work. They did so many tests to see what was causing the nausea but found nothing. Finally, after a year and a half, my doctor said, “You work in one of the most stressful places there is. You need to take your disability leave.” He also said, “You are on uncharted ground. No one survives as long as you have. We don’t know what else to do.” I still hear these words all of the time.
I was very upset about leaving my job because I loved what I did, but I had to do it.
The nausea continued for over 22 years! I was given Zofran, which sometimes helped and other times didn’t. The nausea was really bad and would last for weeks or months. We couldn’t plan to do anything, but I was so thankful to still be here with my husband and family. The pain didn’t matter. I’ve seen and done so many things that I would have missed. You have to realize this is life-altering.
For the last three years or so the nausea has decreased considerably. I started doing yoga in 2018 and I credit that for helping me a lot.
Since my Whipple, I have had a couple of small bowel obstructions. The last was in March 2021 and was caused by so much scar tissue that none of my organs were recognizable. It took over three hours for the surgery to remove the scar tissue.
Living Cancer-Free for 26 Years
For 20 years I returned to my doctor for checkups, CTs, and full body MRIs. So far, so good. I’ve had no other cancer.
My GI doctor now is Dr. Mark Payne at MUSC, who I see every other year. Dr. Tarnasky is now in Dallas, Texas; Dr. Adams is now retired. Dr. Robert Haus was my GI doctor for about 17 years, before Dr. Payne.
Although it is a two-hour drive or a little more from Myrtle Beach to Charleston for us, it has been well worth it. I have lost several friends to pancreatic cancer, including my best friend Vicky. So many people have told me they don’t want to drive even an hour or hour and a half. I don’t understand this. It could save your life.
Going to MUSC in Charleston for a second opinion, at the insistence of my husband Bill, is what saved my life. They are a teaching hospital and do a lot of pancreatic cancer research. I would recommend anyone diagnosed with any cancer to seek a second opinion or even a third or fourth until you are satisfied. A second opinion saved my life!
I was 46 years old when I was diagnosed. I didn’t think I would live to see 47. I am now 72 years old and looking forward to my 26th year as a pancreatic cancer survivor on September 13, 2022! I honestly believe I have a guardian angel, my Daddy.
I am always willing to talk to anyone about my experience. I know some things have changed since my surgery. They still do Whipples, just a little differently. But they are still just as big. I’ve known a lot of friends that have a friend or relative going through pancreatic cancer and have told them to talk with me. I am now talking with my stepsister Becky Reed, from Covington, Virginia, who just had the Whipple but wants no more chemo. She is having difficulty affording her enzymes. This is a problem for many. I also have a friend Janet Kidd, also from Covington, who I am talking with, to give her hope and encouragement.
Please remember to FIGHT and keep faith.