Crafting a Medical Family Tree
It’s no secret that cancers of all types can have a genetic link.
Studies show that about 10 percent of pancreatic cancers have an inherited component. Plus, certain inherited genetic mutations, such as BRCA mutations, can have relevance for a patient’s family members.
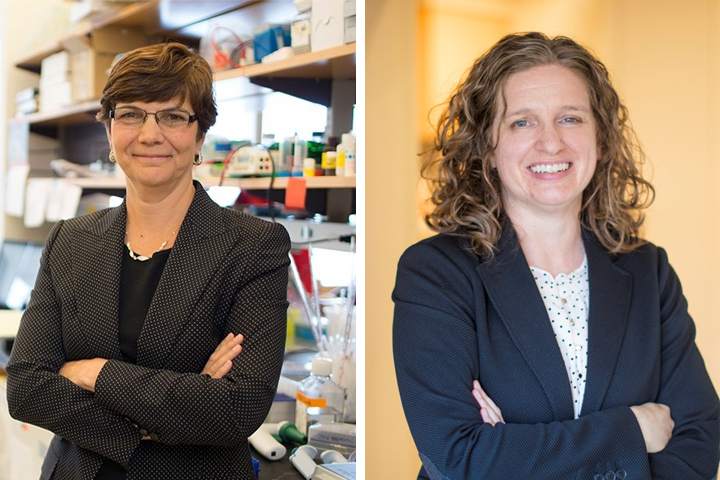
“When you have a family member with pancreatic cancer, it’s critical to ask questions about the rest of the family—who else had cancer, what kind of cancer they had, and how old they were when they had it,” says Diane M. Simeone, M.D., the Laura and Isaac Perlmutter Professor of Surgery and Professor of Pathology at NYU Langone Health in New York.
Even if you have only one close relative with pancreatic cancer, genetic testing is a reasonable next step. The information gleaned could result in early detection of pancreatic or other cancers—and could save lives.
Medical History beyond Cancer
Knowing your family history of disease may prompt you to make lifestyle changes. For example, someone who has a strong family history of heart disease may be more proactive about exercising regularly and adopting a heart-healthy diet. Similarly, uncovering a pattern of cancer within a family history can not only prompt lifestyle changes, but also help guide decisions about screening and early intervention.
In every case, creating a medical family tree can open the door for important conversations about diseases and conditions that affected extended family members. And that’s important, since certain genetic syndromes, such as Lynch syndrome, familial atypical multiple mole melanoma (or FAMMM syndrome), and BRCA mutations, along with hereditary pancreatitis, all increase the risk of developing pancreatic cancer.
So if you have a family member who tested positive for a BRCA mutation, it makes sense to get genetic testing. And if you discover that you, too, carry a BRCA mutation, you may partner with your doctor to develop a more rigorous screening schedule for a variety of cancers, including pancreatic cancer.
“While knowing the full family history is important, people should also know that the National Comprehensive Cancer Center guidelines support genetic testing for anyone with a first degree relative with pancreatic cancer, even if there is no other cancer history in the family,” says Simeone. In fact, about 10 to 15 percent of pancreatic cancer patients have a germline mutation (mutations passed on from parents to offspring) that increases pancreatic cancer risk, even in the absence of a positive family history.
A Family History Tool
People who have a family history of cancer, particularly those who have watched other family members battle the disease, may be afraid to delve into their own personal risk of developing the disease. But understanding your family history and getting the appropriate genetic tests has tremendous benefits.
“If we’re ever going to make a dent in survival for pancreatic cancer, we need to find it early,” says Jessica N. Everett, M.S., C.G.C., Clinical Assistant Professor of Medicine and genetic counselor for the Pancreatic Cancer Center at NYU Langone Health. “It’s especially important to follow people who are at high risk of developing pancreatic cancer because of their family history.”
To help patients determine their risk of developing pancreatic cancer, the Pancreatic Cancer Center, in partnership with the University of Michigan Rogel Cancer Center (Ann Arbor), has developed a pancreatic cancer risk assessment tool. If the tool suggests that you have a high level of risk, you’ll be linked to a genetic counselor and pancreatic cancer specialists at the Pancreatic Cancer Early Detection & Prevention Center at Perlmutter Cancer Center.
“When those patients make it to the door to see us, a lot of them don’t realize that screening is available for pancreatic cancer,” Everett explains. “In addition to more rigorous screening, family members of people with pancreatic cancer may have an opportunity to participate in clinical trials to test promising new blood-based biomarkers for the early detection of pancreatic cancer.”
Research shows that finding cancer at an early stage has a marked effect on survival. Studies also suggest that screening high-risk patients increases the chance of detecting a resectable lesion from 15 to up to 90 percent.
“There’s no doubt that family history testing plays a key role in achieving a better five-year survival rate for pancreatic cancer,” Simeone says. “If we know you’re at increased risk of pancreatic cancer, we can do something about it.”