Urinary Tract Scans Lead to My Diagnosis

- Stage II pancreatic cancer
- BRCA2 gene mutation
- FOLFIRINOX and gemcitabine chemotherapy
- Clinical trial with stem cell transplant
The news of my pancreatic cancer diagnosis came as a shock to me because I had no symptoms.
It was December 2021 and I had gone to the doctor for a urinary tract infection. My doctor ordered a scan to see if I had kidney stones. At age 74, this would not be unheard of. Instead of kidney stones, something more dangerous was found in my abdomen—a tumor in my pancreas. I ended up having more scans, a biopsy, and blood work, including the CA 19-9 blood test. That’s when I found out that I had stage II pancreatic cancer.
BRCA2 Gene Mutation
I started treatment at Massachusetts General Hospital (MGH) in Boston, with oncologist Dr. Colin Weekes. Initially I was given chemotherapy with FOLFIRINOX and gemcitabine. My husband Bob is a communications consultant and had a healthcare client who knew of a clinical trial at Memorial Sloan Kettering Cancer Center in New York. When I first met with Dr. Weekes, he told me the trial was opening at MGH, and he was overseeing it. The trial included two phases of stem cell transplants given four weeks apart along with a combination of melphalan, BCNU, vitamin B12b, vitamin C, and ethanol.
Around the same time, Dr. Weekes learned that I have the BRCA2 gene mutation (I had testing when I had a second diagnosis of breast cancer in 2015). This discovery significantly influenced our treatment plan because it allowed me to participate in the clinical trial.
I immediately signed up for the trial. To qualify for this trial, I had to undergo a series of tests to determine if I was healthy enough to withstand all stem cell processes and the particular regimen of drugs I would be taking.
As part of the trial I had an autologous stem cell transplant. My stem cells were removed, treated, and then replaced via two infusions. All of this had to be done in the hospital. I was in the hospital for two phases for a combined total of 32 days. I had to remain in the hospital so I could be carefully monitored as my immune system was severely compromised. During the treatments, I suffered the typical side effects from chemotherapy, including gastrointestinal issues, nausea, and fatigue. I also had reactions to vitamins B12 and C.
Scans Show No Spread
It’s been ten months since I was first diagnosed. It may be too early to tell, but my initial scans after completing the clinical trial and treatment show no spread of the disease. I return for scans every three months. Besides the good results, the clinical trial provided me with hope and gave my husband and me a much-needed emotional lift.
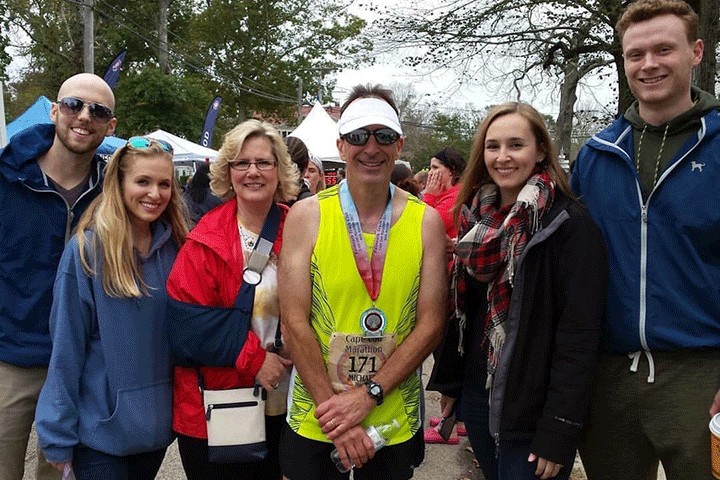
I am enjoying my life now post treatment. Bob and I try to plan an outing or a day trip almost every day of the week. We try to enjoy each and every day and take nothing for granted. Having regained my strength, we plan long walks on paths in the forest or along the ocean. I find being in nature—at the sea or walking through the woods—provides a sense of serenity and helps to calm us both. I still only dine outdoors as advised by my docs, who still want me to be careful. That said, we have been given the “green light” for future trips first domestically and then internationally.