Time and Hope

- Jaundice leads to pancreatic cancer diagnosis
- Treatment on a clinical trial, with chemotherapy and radiation
- Maintenance treatment after
My name is Michael Francis and I am a rose farmer, one of only six in the United States.
My journey with pancreatic adenocarcinoma, better known as pancreatic cancer, began on November 26th, 2018. After a weekend of nausea, at the insistence of my wife I visited my primary care physician with a severe case of jaundice. I was told to go immediately to the Mayo Clinic Hospital emergency room in Phoenix, Arizona.
From the time I entered my doctor’s office to the time I was on the 4th floor of the Mayo Hospital only six hours passed. A CT scan showed a mass in the pancreas that was around blood vessels. I was told that I had stage III pancreatic cancer. A stent was placed in my bile duct the next day and the jaundice disappeared.
Finding Treatment
From there I found myself in an oncologist’s office, where I found out that I was not a candidate for surgery because the tumor was around blood vessels. I was told that my best treatment option was chemotherapy with gemcitabine and Abraxane. He said my median life span would be three years. I asked about clinical trials and was told that Mayo did not have any for locally advanced pancreatic cancer at that time.
My family and I were not happy with this option, so we asked a friend with pancreatic cancer for a recommendation of where to go. My wife’s father and two of her cousins died from pancreatic cancer, so I knew that TGen (in Phoenix) does a lot of research into pancreatic cancer, and works with Virginia G. Piper Cancer Center (VPCC) at HonorHealth, in Scottsdale. I was able to secure an appointment with Dr. Michael Gordon at Virginia Piper. Dr. Gordon took a one-and-a-half-hour personal history from me. His comment at the end was, “I think we can do better than three years.”
On a Clinical Trial
From there I met nurse practitioner Gayle Jameson and entered a phase II clinical trial called NABPLAGEM in December. Working with Dr. Erkut Borazanci, I had chemotherapy with gemcitabine, nab-paclitaxel, and cisplatin for six cycles through April 2019. This was followed by capecitabine and intensity-modulated radiation therapy (IMRT) with radiation oncologist Dr. Steven Sckolnik. This treatment ended on June 17, 2019.
I was still interested in surgery, so I reached out to Dr. Mark Truty at the Mayo Clinic in Rochester, Minnesota, and consulted with Dr. Douglas Evans at the Medical College of Wisconsin (Milwaukee). Dr. Evans explained that surgical removal of the tumor is possible but there is a high risk of side effects because the tumor is around blood vessels.
I had genetic testing but no mutations related to treatment were found.
My Current Status
I am being followed closely by Dr. Borazanci, with CA 19-9 tests and scans every two months. My most recent CA 19-9 level was 66. Scans have shown that the tumor remains stable, with no metastases. I continue to take capecitabine as a maintenance treatment and am also taking vitamin D and metformin, although I do not have diabetes.
I would be remiss if I did not thank the nursing staff at VPCC: Gayle, Paula, Ashley, Dana, Mary, and of course Dr. Borazanci.
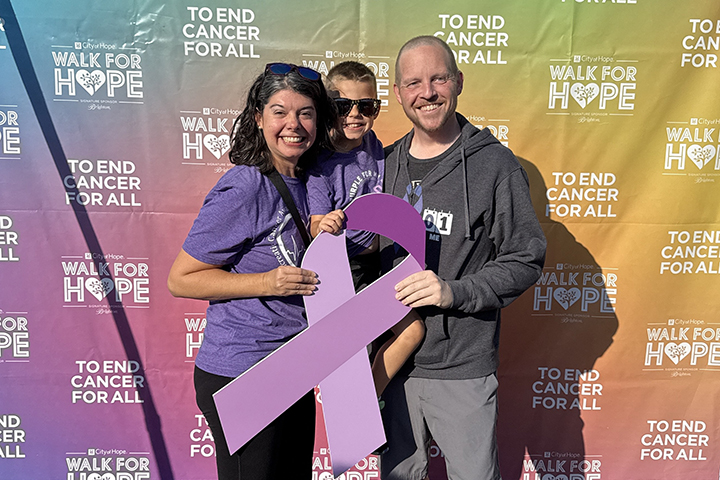
I would not be here without that clinical trial. I am alive, still working on a limited basis, playing golf with my wife, and enjoying life. I am grateful to have TIME and HOPE. TIME to see my grandchildren grow up and HOPE that there is some future.