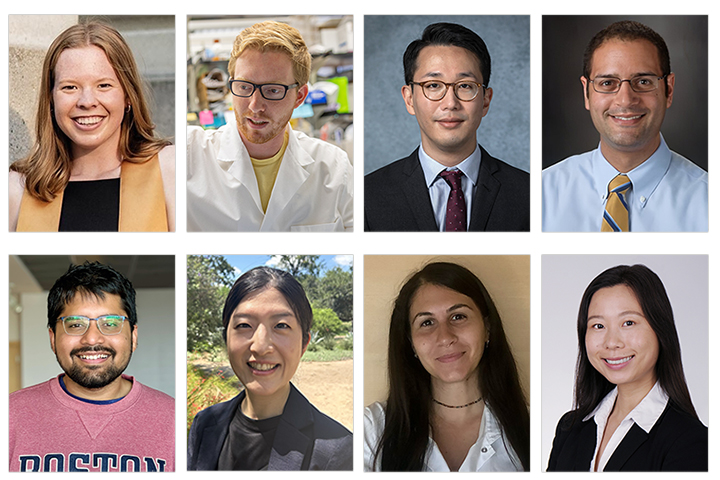
Research: The Next Generation
Science is ever-evolving, building upon prior innovations and breakthroughs to improve our understanding of cancer.
Each generation of researchers brings with them novel ideas on how we can accomplish the ultimate goal of extending lives and even potentially curing pancreatic cancer.
Let’s Win, along with the American Association for Cancer Research, was proud to support the attendance of several scholars-in-training at the 2024 AACR Special Conference: Advances in Pancreatic Cancer Research, held September 15-18 in Boston, Massachusetts. Conference attendance ensures these early investigators will not only be privy to some of the latest breakthroughs in pancreatic cancer, but they will also have the opportunity to meet with established researchers and present their work. Learn how these young scientists hope to make a difference.
Mallory Roach and Jonathan DeLiberty: Inhibiting the Autophagy Pathway
Jonathan DeLiberty and Mallory Roach are currently Ph.D. students in the lab of Kirsten Bryant, Ph.D. at the UNC School of Medicine (Chapel Hill, North Carolina). Roach received her undergraduate degree in cell biology and genetics from Purdue University (West Lafayette, Indiana) while DeLiberty received his undergraduate degree in chemistry with a neuroscience minor from the University of Pittsburgh (Pennsylvania).
Their research focuses on improving how to inhibit the autophagy pathway in pancreatic cancer, which is dependent on both mutant KRAS signaling and autophagy, a metabolic process where a cell can essentially digest its own organelles and proteins and recycle their components in order to survive. When the KRAS signaling pathway is inhibited, pancreatic cancer cells further upregulate this process of autophagy, indicating that it may be helping cancer cells in becoming resistant to KRAS inhibition. While previous work has indicated there is benefit to inhibiting both autophagy and KRAS MAPK signaling, there has been limited success with this combination clinically. By concurrently inhibiting KRAS signaling and the autophagy pathway by treating with two drugs, Roach and DeLiberty have found an effective drug combination to kill pancreatic cancer cells.
Roach credits her high school AP biology teacher who helped her understand how a single mutation in DNA could lead to changes in protein function and eventually cancer. In the future, Roach hopes to transition to an industry position where she can help develop new therapeutics.
DeLiberty knew he wanted to be a scientist from an early age. His mother is a scientist at the University of Delaware, so he grew up with toy microscopes and was able to join his mother at work on occasion. One of his favorite yearly events was helping with Coast Day, an event hosted by the University of Delaware at the Chesapeake Bay that showcased research being done to study and protect the coastal environment; this made him excited to do hands-on research to improve the world. Once he obtains his Ph.D., which he will be defending shortly, DeLiberty hopes to work in biotech, specifically in the early development side of research to continue identifying novel targets and characterizing new drugs in order to develop more effective therapies for pancreatic cancer.
Jaewon Lee: Targeting the Tumor Microenvironment
Jaewon Lee, M.D., currently a surgical oncology fellow at UNC School of Medicine, remembers becoming fascinated with the metabolic pathways and signaling cascades within the cell while working in a lab toward the end of his undergraduate studies at Tufts University (Boston, Massachusetts). Lee received his medical degree from Tufts University School of Medicine, and did his residency in general surgery at Cedars-Sinai Medical Center (Los Angeles, California). He also received additional training as a research fellow at MD Anderson Cancer Center (Houston, Texas) between his second and third years of residency.
At AACR, Lee and colleagues presented an abstract on the cancer-associated fibroblast subtype. Many groups have shown the tumor-intrinsic subtypes are prognostic and potentially have therapeutic value in terms of predicting response to first-line chemotherapies. The cancer-associated fibroblast subtype is newer, without as much data, but given that there is much interest in targeting the tumor microenvironment in pancreatic cancer, the group hypothesized the fibroblast subtypes could predict response to stroma modulating therapies.
To that end, they collaborated with HonorHealth (Phoenix, Arizona), where they conducted a small single-arm trial in which patients were treated with combination cytotoxic therapy (gemcitabine, nab-paclitaxel, and cisplatin) and paricalcitol, which is a vitamin D agonist that may normalize the pancreatic cancer stroma. They knew from applying the fibroblast subtyping to different datasets the fibroblast subtypes can be prognostic for overall survival. They found their treatment regimen normalizes the survival differences between the fibroblast subtypes and the median survival of the more aggressive subtype appears to be prolonged. This opens up the avenue for potential clinical trials where researchers can integrate fibroblast subtypes into stroma modulating therapies.
Lee hopes to become an academic surgical oncologist combining a clinical practice treating patients with gastrointestinal cancers and a translational laboratory program to further study cancer classifiers, with a focus on liquid biopsy platforms.
Vincent Bernard: Assessing the Effects of Radiation on Cancer Cells and the Microenvironment
For Vincent Bernard, M.D., Ph.D., childhood chemistry sets, along with some incredible mentors, spurred his interest in science and the thrill of discovery. Bernard, who is currently a radiation oncology fellow at MD Anderson, received his M.D./Ph.D. through a partnership between the University of Puerto Rico School of Medicine (San Juan) and MD Anderson.
The role of radiation therapy in treating pancreatic cancer is evolving. It can improve local disease control, especially in cases where surgery is not an option, but identifying which patients benefit the most has been challenging. In the study presented at AACR, Bernard and colleagues analyzed a unique set of pancreatic cancer tissue samples to assess the effects of radiation on both cancer cells and the tumor microenvironment. Using advanced techniques like single-cell RNA sequencing and spatial transcriptomics, they discovered that cancer cells surviving radiation show alterations in fatty acid and metal metabolism, revealing new potential therapeutic targets to use in combination with radiation therapy. Furthermore, their findings suggest that radiation uncovers targets against immunosuppressive cells, offering the potential to shift the immune response toward a more pro-inflammatory, antitumor state. These insights could help guide future trials that combine immunotherapy with radiation to improve treatment outcomes.
Bernard’s ultimate goal is to become a physician–scientist in radiation oncology, leading his own research lab while also caring for GI cancer patients, with a focus on pancreatic cancer.
Chaitanya Parikh: Local Delivery of mRNAs
Chaitanya Parikh is currently a fourth year Ph.D. student at Ruscetti Lab at the UMass Chan Medical School (Worcester, Massachusetts). He received his bachelor’s in biotechnology from Vellore Institute of Technology, India, and his master’s in biotechnology from Texas A&M University (College Station).
Parikh says coming from a family of nonscientists, his path into research was deeply personal, motivated by the loss of a close relative who maintained a healthy lifestyle, but still developed and then died from cancer. This experience, he says, sparked a profound curiosity as to why cancer forms and why in some cases it’s so tough to cure.
His mentor Marcus Ruscetti and colleagues previously identified a three-drug combination that triggered an immune response against KRAS mutant pancreatic cancer in mice. However, toxicities associated with the three-drug combination limit its clinical translation. To address this, Parikh and colleagues explored the underlying immune mechanisms and found that these drugs induced the secretion of pro-inflammatory cytokines and chemokines that are important for attracting and activating immune cells in tumors.
Using mRNA technology, they delivered cytokine-encoding mRNAs directly to tumors, leading to significant immune activation, tumor control, and extended survival in mice, even with just one dose. They are now enhancing this approach by combining cytokine mRNAs with antigen mRNAs and immune checkpoint inhibitors like anti-PD-1, immunotherapies currently being tested in the clinic. This is important because local delivery of mRNAs directly to the tumor mitigates the risk of off-target toxicities—a major concern with many current therapies—and it may also improve immunotherapy regimens that so far have not proved viable in pancreatic cancer.
Akiko Sagara: A Better Understanding of IPMNs
Akiko Sagara, M.D., Ph.D., a post-doctoral fellow at MD Anderson’s Maitra Laboratory, decided to pursue medicine in high school, since she was always drawn to a career that would allow her to help people. Born and raised in Japan, she received her M.D. at the Kyushu University School of Medicine and her Ph.D. at the Graduate School of Medical Sciences, both at Kyushu University (Fukuoka City, Japan), where she focused on developing therapies targeting the stroma in pancreatic cancer. Sagara devised a drug screening system aimed at inhibiting the activity of pancreatic stellate cells, which are abundant in the stroma.
Her research focuses on the functional consequences of recurrent RNF43 loss in intraductal papillary mucinous neoplasms (IPMNs), which are cystic precursor lesions of pancreatic cancer. She uncovered a novel mechanism through which RNF43 loss drives metabolic reprogramming in IPMNs, creating increased mitochondrial biogenesis and OXPHOS dependency. This is largely attributed to an upregulated level of IRE1, which localizes at MAM to promote ERMCS formation. These findings highlight a potential therapeutic vulnerability in precursor lesions.
Sagara’s passion for pancreatic cancer research started when she was a surgical resident and saw patients with advanced pancreatic cancer. Her time with these patients profoundly influenced her, leading to a commitment to focus on early detection of and therapeutic intervention for pancreatic cancer, since these are keys to improving patient outcomes.
Sagara aims to establish herself as an independent physician–scientist, integrating research and clinical practice to deepen the understanding of pancreatic cancer and contribute to the development of more effective treatments.
Vasiliki Liaki: Refining Targeted Therapies
Vasiliki Liaki, Ph.D., specializes in molecular therapeutics of pancreatic cancer. She completed her Ph.D. studies in the Spanish National Cancer Research Center (CNIO) in Madrid, Spain, under the supervision of Professor Mariano Barbacid. Currently, as a junior postdoctoral fellow, she focuses her activity on KRAS inhibitor resistance. She also investigates the molecular mechanisms of metastatic pancreatic tumors, aiming to develop more combined targeted therapies.
Liaki, a native of Greece, obtained her undergraduate degree in biology from the National and Kapodistrian University of Athens. Prior to joining her current lab in CNIO, she completed her master’s degree at the University of Cologne (Köln, Germany), where she specialized in genetic mouse models and mechanisms of DNA damage response under the supervision of Professor Christian Reinhardt.
She and colleagues have developed a novel targeted therapeutic strategy against the signaling network of the KRAS oncogene, targeting the expression of EGFR, RAF1, and STAT3, leading to complete regression of pancreatic tumors in preclinical models using genetic and pharmacological approaches.
In the future, she would like to remain part of the academic community, working in close collaboration with the pharmaceutical industry. With her training in bioinformatics and knowledge of how to translate big data to targeted therapies, Liaki eventually would like to be able to validate the efficacy of targeted pharmacological combinations in different preclinical models of pancreatic cancer.
She credits her father, a physics teacher, as well as her high school biology teacher, with helping her hone her early interest in the sciences.
Lu Han: New Insights Into Pancreatic Cancer Associated Fibroblasts
Lu Han, Ph.D., is pursuing postdoctoral studies in cancer biology at the Medical University of South Carolina (Charleston), where she also serves as an assistant professor. She did undergraduate studies in biotechnology at China Pharmaceutical University (Nanjing), and received her Ph.D. in developmental and molecular biology from the University of Cincinnati (Ohio).
Her research work focuses on pancreatic cancer associated fibroblasts, which are a particular type of cells surrounding the pancreatic cancer cells. She investigates how certain fetal developmental principles can regulate how fibroblasts interact with cancer cells. A better understanding of these interactions may uncover novel ways to combat cancer formation by changing how fibroblasts interact with cancer cells.
Han studied cell–cell interactions during fetal organogenesis during her Ph.D. thesis work and became fascinated by how cell interactions are well orchestrated and essential for biological processes. She pursued this interest in the context of cancer in the pancreas, which is one of the organs derived from the embryonic structure that she studied during her Ph.D.
In the future, Han would like to perform in-depth research as to how developmental principles regulate fibroblasts in the pancreatic cancer microenvironment. And she would like to mentor three or four Ph.D. graduate students or postdoc fellows.