Aiming to Improve Immunotherapy for Pancreatic Cancer

Despite the increase in longer-term survival, it is clear to physicians and patients battling pancreatic cancer that more effective treatments are desperately needed.
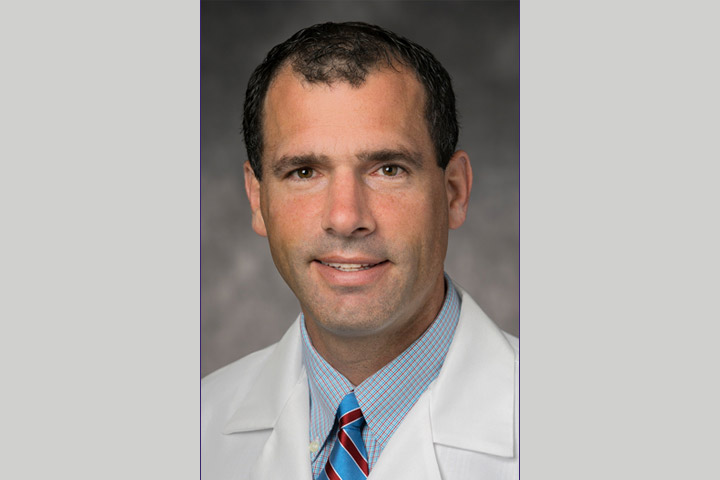
One particular area of interest: improving immunotherapy, a treatment that has shown to be effective in many cancers but, so far, not pancreatic cancer. “We can’t obviously be satisfied with the status quo and I think that the field needs to redefine what it means in terms of meaningful advances,” says medical oncologist Dr. Deirdre Cohen, Director, Clinical Trials Office at NYU Langone’s Perlmutter Cancer Center. “Immunotherapy is one area that’s very exciting, but we just need to figure out how it may be able to work for pancreas cancer.”
Cohen and colleagues are particularly excited about a new multi-site trial combining nivolumab, cabiralizumab, and stereotactic body radiation therapy (SBRT) in patients with locally advanced pancreatic cancer that cannot be surgically removed (unresectable). About half of patients with pancreatic cancer present with regionally advanced disease. This includes borderline resectable and locally advanced unresectable tumors. Chemoradiation (chemotherapy plus radiation) is used in this setting in an attempt to control local disease and possibly shrink the tumors so they can be removed.
In this phase II study, researchers will determine the safety and tolerability of this three-pronged approach—combining two immunotherapy drugs with targeted radiotherapy. They will also estimate the surgical resection rate after treatment. “Surgery is the only potentially curative option for patients right now, so if some tumors become more amenable to surgery after this approach, that’s a win,” says Cohen, who is also an Associate Professor of Medicine, NYU School of Medicine.
Boosting the Power of the Immune System
Some early research is showing some promise in combining nivolumab with cabiralizumab, both of which are immunotherapy agents. Nivolumab is a monoclonal antibody or checkpoint inhibitor that helps direct the body’s immune system to attack tumor cells. It targets PD-1, a checkpoint protein on immune cells called T cells, the body’s natural defense. Cabiralizumab is also a monoclonal antibody. It blocks the colony stimulating factor 1 receptor (CSF1R), which is found at the surface of immunosuppressive tumor-associated macrophages (TAMs). TAMs help tumors progress by suppressing the ability of immune system T cells to kill tumor cells. High levels of TAMs are often linked with poor prognosis.
A small phase I study showed that combining these two immunotherapy agents could provide some help for metastatic pancreatic cancer patients. The results of the study were presented at the Society for Immunotherapy of Cancer conference in 2017. At the time of the presentation, four out of 31 heavily-pretreated pancreatic cancer patients had responded to the combination therapy. The therapy appeared to shrink the tumor in these patients, as well as reduce the levels of certain proteins found in the blood that are correlated with the volume of cancer in the body.
Radiation, which hasn’t proven all that effective in pancreatic cancer, is often used for patients with locally advanced disease. By adding radiotherapy into the mix, the NYU Langone researchers hope to boost the chances of immunotherapy being more effective. “That idea (for the trial) came from the lab of (Dr.) George Miller and colleagues who found that if you block macrophages with an antibody, you improve the chances of radiation being more effective in slowing tumor growth,” says Cohen, the lead investigator of the trial. (Miller is a hepatobiliary surgeon and principal investigator and director of the S. Arthur Localio Laboratory in NYU Langone’s Department of Surgery.)
To learn more about the trial, visit the page on ClinicalTrials.gov.
Another Immunotherapy Trial for Pancreatic Cancer Patients
In collaboration with scientists at GlaxoSmithKline, NYU Langone researchers (along with researchers at other sites) will be studying the efficacy of a new drug called GSK3145095, in another clinical trial. The agent works by blocking the action of an enzyme called receptor-interacting serine/threonine-protein kinase 1, or RIPK1, which regulates macrophages. Early research showed that treatment brought about a doubling of killer T cell activation and a fivefold decrease in the macrophage-influenced T cell type that suppresses the immune system, according to research published in the journal Cancer Cell.
“This work also came out of the (Miller) lab and we’re very excited about it because it may show that if we can inhibit RIPK1 we can potentially make a pancreas tumor, as well as some other solid tumors, better targets for immune checkpoint modulators,” says Cohen, who will also lead this trial.
If pancreas cancer treatment is to improve, Cohen believes these types of trials offer the best chance to “move in the right direction.” “I love my patients, but I think that can be said of all doctors. There is, however, a special quality to patients with GI cancers. These patients face their disease in the most courageous way, and pancreas cancer is specifically challenging and heartbreaking. We need to do better and the way to do better is to quickly get from the lab into trials to see what works. That’s how we can improve the lives of our patients.”