A Potential Role for PARP Inhibitors in Pancreatic Cancer
Just a few years ago, pancreatic cancer was the fourth leading cause of cancer deaths in the U.S.
Due to numerous factors, including rising rates of obesity and smoking, for example, pancreatic cancer jumped to number three, and some researchers predict it will soon be number two in terms of cancer deaths.
What’s clear is that better treatments are needed. Fortunately, scientists are making some progress with targeted therapies like PARP inhibitors, which have already changed the treatment landscape for some patients with solid tumors such as ovarian and breast cancer. The hope is that eventually, PARP inhibitors may prove to be as effective in the treatment of pancreatic cancers.
What Is a PARP inhibitor?
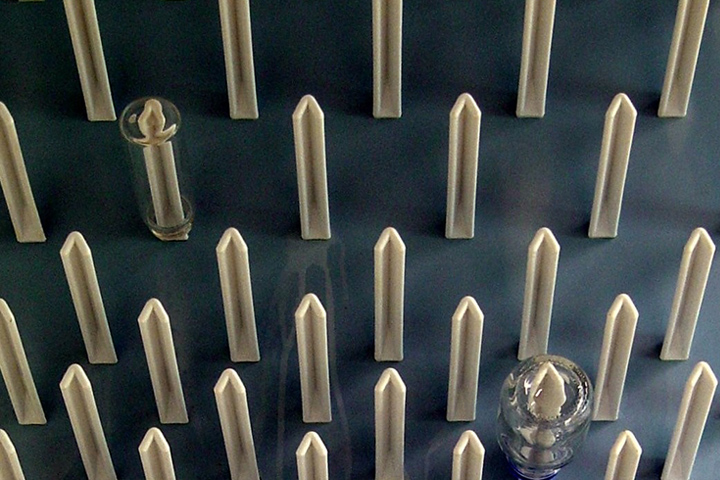
Targeted treatments are selected by doctors based on the specific genetics of a patient’s tumor. PARP, or poly (ADP-ribose) polymerase, is an enzyme found in our cells. Its job is to help damaged cells repair themselves.
The goal of a PARP inhibitor is to stop PARP from doing its repair work; this leads to multiple double-strand DNA breaks to form. In patients who have homologous recombination deficiency (HRD), such as mutations in the BRCA gene, their cells are unable to repair these double- stranded breaks, and thus cannot survive, explains gastrointestinal oncologist Dr. Michael Pishvaian. He has been studying PARP inhibitors for more than a decade for potential use in gastrointestinal cancers such as pancreas or colorectal cancers.
The best-known HRD pathway regulators are the so-called breast and ovarian cancer genes BRCA1 and BRCA2, which are tumor suppressors. Mutations in these genes can be tumor only (somatic) or inherited (germline.) Germline mutations are genetic abnormalities that are passed on from parents to offspring. BRCA-related ovarian cancers, for example, make up about 15 percent of all ovarian cancers diagnosed in the United States, and patients with these BRCA mutations have up to a 60 percent lifetime risk of developing ovarian cancer.
“What we know is that tumors with BRCA mutations are prone to double-strand DNA breaks,” says Pishvaian, who is the Director of the Phase I Clinical Program, and Co-Director of the Ruesch Center Pancreatic Cancer Program at Georgetown University’s Lombardi Comprehensive Cancer Center. “So if you give a PARP inhibitor to a patient with a BRCA mutation, repair of the DNA damage becomes very inefficient. Tumor cells die and normal cells are spared.”
PARP and Pancreatic Cancer
About 3 to 5 percent of pancreatic cancer patients also carry mutations in the BRCA genes. But there is also a concept called BRCAness, which involves mutations in other key BRCA-related genes such as PALB2, ATM, or CHK2. “When you look at other genes that have a BRCA-like phenotype, the target population for PARP in the pancreatic cancer setting could be as high as about 17 percent, thus expanding significantly the population of pancreatic cancer patients who could benefit from therapies like PARP inhibitors,” Pishvaian explains.
Pancreatic cancer patients with BRCA and BRCA-like mutations also seem to have improved survival rates with platinum-based chemotherapies, so researchers are also studying PARP inhibitors combined with a platinum-based therapy.
“When we look at the patients with BRCA mutations, what you have is FOLFIRINOX as one option or gemcitabine/cisplatin, but after a few months of therapy, patients are wiped out and tired,” Pishvaian says. “So one question we want to answer is, can these patients be put on a single-agent PARP inhibitor once the disease is actually controlled. We don’t know that yet, so it’s clear that we need to do more research, because it would be a great benefit to patients.”
PARP Inhibitors and Clinical Trials
Numerous pancreatic cancer PARP inhibitor-based trials are looking at multiple PARP inhibitors, such as olaparib, rucaparib, and veliparib. One study called POLO is a randomized Phase 3 trial for stable metastatic pancreatic cancer patients with BRCA or PALB2 defects. Its goal is to determine whether giving olaparib to people with metastatic cancer of the pancreas can help to control the disease between chemotherapy treatments. To test the effectiveness of a new combination of drugs, another study, led by Pishvaian, is looking at veliparib in combination with 5-fluorouracil and oxaliplatin (modified FOLFOX-6) in patients with metastatic pancreatic cancer.
Pishvaian is hopeful that these and other PARP inhibitor-based trials will provide more clues as to how they may be most effective. “We don’t have good maintenance approaches for pancreatic cancer and we clearly need better treatment,” he says. “PARP inhibitors may turn out to be part of an overall treatment plan.”
While researchers are still piecing together data on how best to use PARP inhibitors, one thing is clear: pancreatic cancer patients should consider molecular profiling of their tumors, Pishvaian emphasizes.
“The more we learn about pancreas cancer, the more we realize that effective treatment approaches need to be individualized, and a molecular profile will give the patient and the doctor more information about that specific tumor,” he says.
“If you know more about the tumor you can hopefully better target treatment options, including recommending a PARP inhibitor-based trial. Patients need more options than what we can offer today.”