Finding a Treatment Geared to My Cancer
- Initial treatment with FOLFIRINOX and radiation
- Looking for alternatives that might work better
- Switched to treatment designed for his cancer
- Surgery is the goal
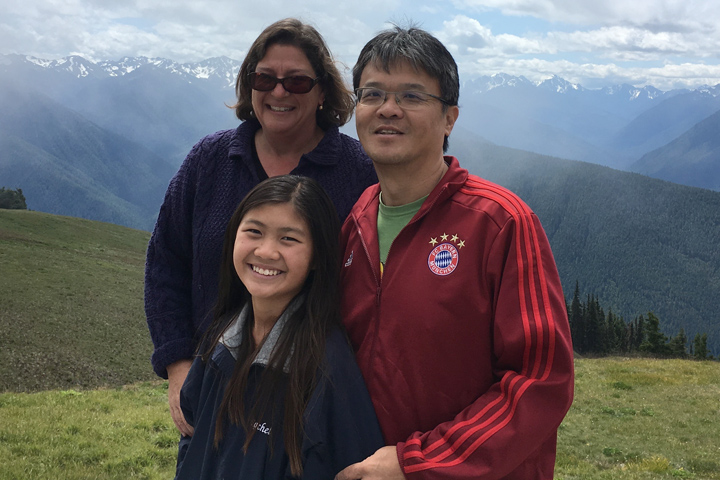
The call from my general practitioner came while I was driving my then 10-year-old daughter home from art camp. I kept my cool as my doctor told me that it was likely I had pancreatic cancer.
Within a couple of hours, my wife and I were in our doctor’s office and he reviewed with us the results of an MRI he had ordered. I had been experiencing stomach pains and digestive problems for a few weeks. It was the afternoon of July 22, 2015; I had the MRI that morning. It was the second imaging test I’d had in six months. The first, a CT scan in January 2015, did show something “suspicious,” but my doctor treated me with antibiotics and the pain went away. Too bad.
Our doctor referred us to University of California, San Diego Health (UCSD), where I underwent a biopsy, which confirmed an adenocarcinoma of the pancreas. The only good news was that the cancer was localized, though it had already grown out of my pancreas to involve several arteries and veins.
Starting Standard Treatment
UCSD was very efficient. The following week, I had a “Smart Port” installed and in early August, I began chemotherapy. The protocol was FOLFIRINOX and the goal was to shrink the tumor enough to make it operable.
I had awful side effects from the FOLFIRINOX. But despite a notable weight loss, I did feel well enough to continue working, riding my bike, and walking. I went through about six rounds of FOLFIRINOX and then FOLFOX (the irinotecan was eliminated) before a second scan showed little progress. By October, my doctor suggested we search for second opinions.
Looking at Other Options
After trips to University of California, San Francisco—to meet with Dr. Andrew Ko, who was working on a clinical trial with CAR T cells—and MD Anderson Cancer Center (Houston) for a full work up and second opinion, radiation was recommended. Dr. Milind Javle at MD Anderson felt proton beam therapy would be most appropriate; however, I was not a candidate. Dr. Javle did, however, answer many questions and was the first doctor to really review my scans with me. He showed me that the tumor had, in fact, shrunk between August and October. My wife also consulted by phone with Johns Hopkins and several specialty surgeons. However, all felt surgery was not an option at that point.
I continued to have chemotherapy through this time and had a final round in mid-January before beginning a five-week daily course of radiation therapy at UCSD. Despite my expectation that radiation would be more tolerable than chemotherapy, it was not.
A Personalized Treatment Plan
Throughout all of this, my wife had begun researching Dr. William Isacoff, a pancreatic oncologist in Westwood, California. She found Dr. Isacoff almost by mistake—a patient of an herbalist that a friend used suggested we contact a surgeon in Philadelphia. Upon doing so, a nurse in the office mentioned Dr. Isacoff. My wife began researching and discovered Dr. Isacoff seemed to have more success than more mainstream, institutional doctors. He subscribes to the idea of treating patients with low-dose chemotherapy—using the minimum amount of medicine required for results rather than the maximum tolerable dosage—alongside cutting-edge tests.
My wife spoke with Dr. Isacoff one morning before I was to have a round of radiation. She relayed Dr. Isacoff’s directive: “Handcuff Sam to the car and bring him to me. Tell him that the radiation will only weaken his system so he won’t be able to tolerate chemotherapy, which is what will really help.” I called UCSD that morning and cancelled the rest of my radiation.
Within a few weeks, I was being treated by Dr. Isacoff. He ordered a “chemosensitivity” test, performed by Dr. Mark Ricigliano. The blood test essentially matches chemotherapy drugs to one patient’s tumor. It is a roadmap that Dr. Isacoff can use in ordering chemotherapy. He also ordered a blood test to determine if I had any gene mutations (I don’t) and a urine test to look at the KRAS gene. None of these tests are in wide use, and all are helping to guide my treatment.
The change in how I feel with the new treatment is dramatic. Though I often have a one-week portable 5-FU IV pack, my side effects are fewer, less intense and less frequent. I have been treated over the last seven months with 5-FU, cisplatin, gemcitabine, and mitomycin-C. I continue to work full-time, cycle, walk, attend my daughter’s events and take family vacations. Four months after starting with Dr. Isacoff, my scan showed a reduction in the size of my tumor.
Future Steps
During this time, I’ve also been in touch with a surgeon at the Mayo Clinic in Rochester, Minnesota, who is doing cutting-edge procedures—vascular reconstruction along with removal of pancreatic tumors. I will visit the Mayo Clinic for preliminary tests in January and am hopeful I will be a candidate for this procedure.
Overall, I’ve been able to find the best doctors for me, who are doing cutting-edge work and who believe that I have future. Dr. Isacoff is not just concerned with how I am handling treatment, but what comes next. And both he and the surgeon I am in contact with are strong believers in the idea that chemotherapy is a critical part of beating pancreatic cancer. The more chemotherapy I can have (as unpleasant as that is), the healthier I should be in the long run.
I am grateful to have found Dr. Isacoff—and all of the talented people he is associated with. I will continue to fight this beastly disease until it is eradicated from my body.
Samuel passed away from pancreatic cancer after his story was published. We deeply appreciate that he shared his story with Let’s Win, so that other pancreatic cancer patients could learn about the different treatments that are available.