Working With your Doctor to Find Clinical Trials
Daniel Sone, National Cancer Institute, National Institutes of Health
As oncologists, we are trained to use the information in front of us to make decisions about the best treatments for our patients.
How healthy is the patient? What other medical problems does he or she have? What is the extent of his disease? What are her personal wishes? What is the most recent literature on the available treatments?
We rely heavily on clinical trials conducted by ourselves and our colleagues, particularly when a patient has a hard-to-treat form of cancer. Some trials are very large, well-constructed studies that give us confidence in our treatment choices. But often enough, there have only been small, scattered trials on various therapies. Sometimes there is no data at all that matches a specific situation.
Thinking Creatively About Treatments and Clinical Trials
For pancreatic cancer, the treatment picture is murky. Historically, the available therapies for pancreatic cancer have not been nearly as effective as we need them to be. Because of this patients and physicians must think creatively and carefully about each treatment decision. Standard-of-care therapies are certainly an important part of treatment, but doctors and patients should carefully evaluate additional options at every stage.
It is important to realize that all pancreatic cancers are not the same. Most are sporadic, meaning they arise randomly without a discernible cause. Others are caused by mutations in genes. These mutations can be passed down in families or they can occur spontaneously. We are learning every day that looking closely at individual patients and their tumors can lead us to therapy that is more closely targeted to that individual.
The Importance of Family History
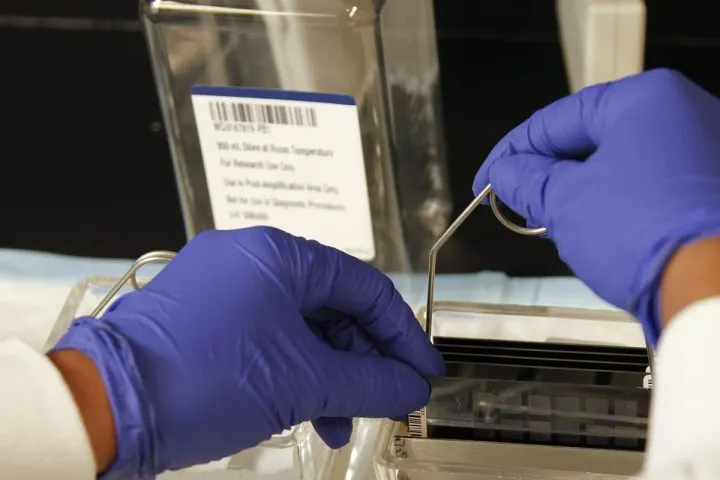
Taking a family history of cancer is an important first step. The family history may uncover clues that the tumor is linked to a specific gene or syndrome. Sequencing of tumor tissue, which uses laboratory techniques to look at the genetic make-up of a patient’s specific cancer, can also sometimes turn up a mutation for which a drug may be approved and available. Or, the patient may qualify for an available clinical trial.
These types of tailored approaches are often, though not always, more readily offered at academic medical centers. Large academic centers are driven by research and therefore may have access to cutting-edge technology and science. In addition, the oncologists at academic centers are focused on one or a small cluster of diseases. This means that the oncologist you would see at an academic center spends all of her time studying your disease. As such, she will have a higher chance of knowing the latest information.
What to Do
As a newly-diagnosed patient, what should you or a family member do?
First, if you have a family history of cancers (even if they are not pancreatic cancer), make sure your oncologist knows about it.
Second, ask about tumor sequencing and testing for microsatellite instability (MSI), a rare but important finding that may mean your tumor might respond to immunotherapy. The genetics of your tumor can help determine which treatment to pursue, and what might not be effective.
Third, find out about clinical trials. No one doctor can know all the trials available, but information is available online. Another way to find out about trials is by networking with the various organizations that follow current clinical trials. These groups will help you find information. The National Institutes of Health and Pancreatic Cancer Action Network each maintain searchable databases on the internet, at ClinicalTrials.gov and Let’s Win Trial Finder, respectively. When you find a clinical trial you are interested in, take the information to your oncologist and talk it through with your medical team. Consider whether a trip to an academic medical center for a second opinion might be worth your time.
Together, you can work to find the best therapies to fit your cancer and your health needs.
Kim A. Reiss, M.D., is an oncologist at the Abramson Cancer Center, at the Hospital of the University of Pennsylvania in Philadelphia.