Does it Run in My Family?
The connection between your family’s medical history and pancreatic cancer
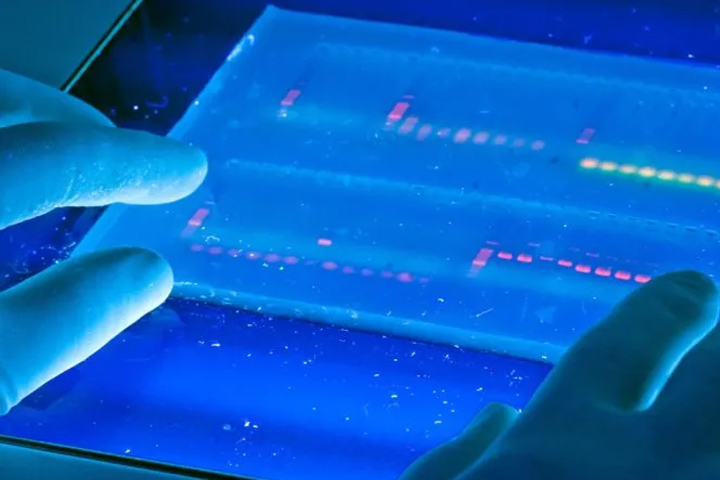
As you may already know, cancer can run in families. In fact, people carrying certain genetic mutations have an increased risk of getting cancers including breast, colon, prostate, ovarian, and pancreatic cancer. All told, researchers estimate that known genetic mutations are related to roughly 10 percent of cases of pancreatic cancer. But there are also families with a striking number of pancreatic cancer cases, but no known mutation.
The mutation most often found when there is a family history of cancer is in the BRCA gene. If you’re familiar with BRCA1/2 mutations, you may likely think of them as causing breast cancer. But BRCA mutations—in particular BRCA2—can also increase your risk for developing pancreatic cancer. In fact, BRCA2 mutations increase your risk more than all the other cancer-related mutations, accounting for 5 to 17 percent of all inherited pancreatic cancers.

Learn more about BRCA
The Basser Center for BRCA is the first comprehensive center for the research, treatment, and prevention of BRCA-related cancers, including breast, ovarian, pancreatic, prostate, and melanoma.
But BRCA mutations are not the only ones that increase pancreatic cancer risk. Scientists call PALB2 a “pancreatic cancer susceptibility gene” because it makes you more likely to get the cancer, although how much more likely is not yet known.
There are other cancer-related conditions that can run in your family and thus increase pancreatic cancer risk, too. These include Lynch syndrome-related colorectal cancer (MLH1, MSH2, MSH6, and PMS2), Peutz-Jeghers syndrome- related digestive system cancers (STK11), hereditary pancreatitis (PRSS1), familial atypical multiple mole melanoma (FAMMM) syndrome, and ataxia-telangiectasia (ATM), a cerebellar degeneration syndrome.
But genetic mutations are just one piece of the complicated inherited pancreatic cancer puzzle. Another five percent of pancreatic cancers occur in families that have a history of the disease but no known mutation. It is not clear if these families have a yet-to-be-identified mutation or if another factor is involved. This is why family medical history is so important.
What You Can Do
The first step is to learn your family medical history. Has anyone had cancer in your family? If so, what kind? Does a particular type of cancer run in your family? Does it include pancreatic cancer? Make it a point to ask your parents, grandparents, aunts, uncles, and siblings for that important information. Then share what you learn with everyone, especially your children.
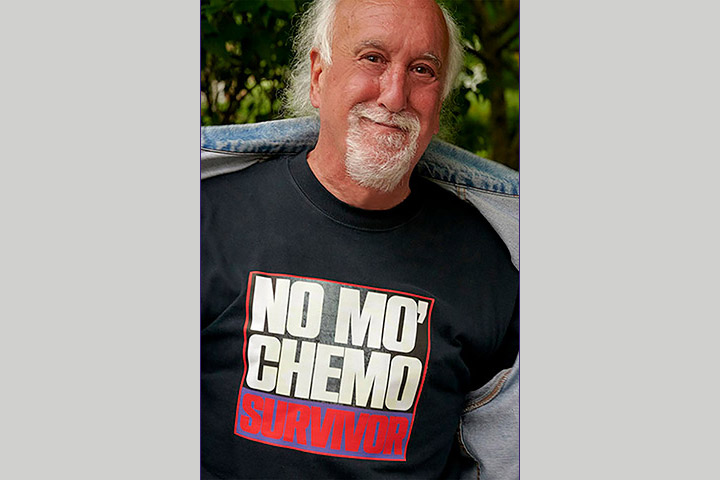
A Cancer-Free Life 25 Years in the Making
Andy Lyons lost many family members to pancreatic cancer. With such a family history he knew to be proactive and get screened regularly.

Family History Matters
After Martin Abrams lost two siblings to pancreatic cancer, he made sure he was screened regularly because of his family history.

My Journey with Pancreatic Cancer
Dr. Robert Wagar lost both parents to pancreatic cancer. When his wife found an article about a surveillance study he had an MRI, which found a lesion.

Pancreatic Cancer and Family History
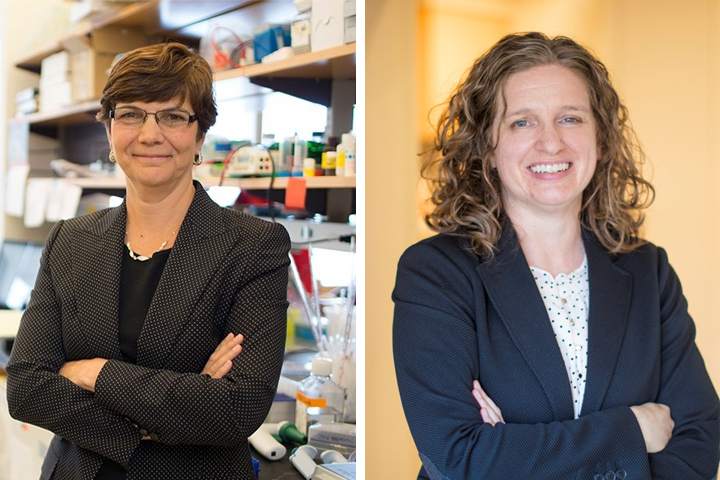
Dr. Diane Simeone is developing a tablet-based family history survey to identify patients with a genetic-based risk for developing pancreatic cancer.
Crafting a Medical Family Tree
Dr. Diane Simeone and genetic counselor Jessica Everett explain why it is important to create a medical family tree for pancreatic cancer.
Learn About Genetic Testing
If your family has a history of cancer, particularly breast, ovarian, prostate, or pancreatic, you should consider making an appointment with a genetic counselor. The counselor can guide you through the testing process and help you understand the results.
Knowing that you carry a mutation such as BRCA also helps other family members. They can also get tested, and those who carry the same mutation can manage their risk by participating in screening programs.
Genetic testing also impacts treatment. Carriers of the BRCA and PALB2 mutations respond better to certain chemotherapy drugs and targeted treatments such as PARP inhibitors. In fact, genetic testing is now standard of care for pancreatic cancer patients, meaning that all patients should get tested.

Decoding the Differences between At-Home and Medical Genetic Testing
Genetic counselors Jill Stopfer and Heather Hampel explain the differences between at-home and medical genetic testing, including precision and knowledge.

Genetic Testing for All Pancreatic Cancer Patients
A study by Dr. Gloria Petersen’s research team has led to an official recommendation that all pancreatic cancer patients get genetic testing.
The ABCs of Genetic Testing
There are a number of different genetic mutations that can cause familial pancreatic cancer. This article explains some of the most common ones.
Before You Leap: Genetic Testing for Pancreatic Cancer
Genetic counselor Megan Frone outlines the advantages of genetic testing when there is a family history of pancreatic cancer.

Improving Access to Genetic Testing and Counseling
Dr. Angela Bradbury is leading a study on access to genetic testing and genetic counseling, including a telehealth option.

Studying One Family’s Mutations May Change Pancreatic Cancer Treatment and Prevention
Dr. Sahar Nissim is studying the genetic mutations in one family predisposed to pancreatic cancer, to find new ways to combat the disease.

Genetic Testing Can Help Those You Love
Dr. Fay Kastrinos, director of the Muzzi Mirza Pancreatic Cancer Prevention and Genetics Program at Columbia University Medical Center, explains the value of genetic testing for cancer prevention and treatment.
Understanding a Family’s Risk for Pancreatic Cancer
A tumor registry studies the genetics of pancreatic cancer to determine risk factors for families.
Screening Programs
Until a definitive test for early detection of pancreatic cancer is available, screening people at higher risk is the best way to diagnose pancreatic cancer at its earliest stages.
If you have a family history of pancreatic cancer or have one of the mutations that increase your risk of the disease, you may want to consider joining a screening program. Many cancer centers screen people at high risk as part of their overall cancer programs. There are also clinical trials that study people with a family history of pancreatic cancer, for example the CAPS5 study and the PRECEDE trial. Screening programs around the country include:
- NYU Langone Health Perlmutter Cancer Center: Pancreatic Cancer Screening
- Mount Sinai Pancreatic Cancer Early Detection Consortium
- UC San Diego Health, Moores Cancer Center: Pancreatic Cancer Prevention
- UVA Health High Risk Pancreatic Cancer Screening Clinic
- Cedars-Sinai Pancreatic Cancer Screening
- Vanderbilt High Risk Pancreatic Cancer Surveillance
- Roswell Park High-Risk Pancreatic Cancer Screening
- OHSU Brenden-Colson Center Pancreatic Cancer High Risk Clinic
- Froedtert & the Medical College of Wisconsin Clinical Cancer Center
- Abramson Cancer Center Pancreatic Cancer Risk Management
- Marshfield Clinic Health System High Risk Pancreatic Cancer Screening Program
- Yale Medicine Pancreatic Cancer Early Detection
- UChicago Comprehensive Cancer Center Early Detection Program
- Hoag Anita Erickson Pancreatic Cancer Early Detection Program
- Columbia University Pancreas Center: Muzzi Mirza Pancreatic Cancer Prevention & Genetics Program
Tumor registries look for risk factors, genes, and biomarkers that could be used for early detection tests. The registries are open to current patients and family members and include surveillance programs for participants.
- Memorial Sloan-Kettering Cancer Center Pancreatic Tumor Registry
- The National Familial Pancreatic Tumor Registry
- Jefferson Health, Jefferson Pancreas Tumor Registry (JPTR)
- OHSU Brenden-Colson Center, Oregon Pancreas Tissue Registry

Who Should Be Screened For Pancreatic Cancer
Who should be screened for pancreatic cancer? Dr. Allyson Ocean explains how genetic mutations and family history factor into screening.

Screening Programs Save High-Risk People
Dr. Michael Goggins explains who should undergo regular pancreatic cancer screening and where programs can be found.

Putting Familial Risk In Perspective
Dr. Alison Klein works to understand the relationship between familial risk and the chances of developing pancreatic cancer.

Understanding Who Is at High Risk for Pancreatic Cancer
Who is high-risk for pancreatic cancer? Oncologist Dr. Matthew Yurgelun explains high-risk populations and what steps to take if you meet the criteria.

Younger Brother’s Pancreatic Cancer Leads to Regular Screening for his Oldest Brother
When Scott Nelson was diagnosed with pancreatic cancer, oldest brother Steve began regular screening, which lead to his early diagnosis.

Which Is the Best Screening Method for Pancreatic Cancer?
Dr. Aimee Lucas outlines the pros and cons of various screening methods that can be used for pancreatic cancer, and who should be using them.

Early Detection Makes All the Difference
Carolynn Kiel lost her mother and sister to pancreatic cancer. Regular screening allowed early detection of her pancreatic cancer.
Resources
Let’s Win and organizations such as the Basser Center for BRCA and the American Society of Clinical Oncology have a wealth of information about the relationship between genetic mutations, family history, and cancer. Learn more about the guidelines for who should consider genetic testing and pancreatic cancer screening.
New Gastrointestinal Screening Guidelines for High-Risk Patients
Get informed about the latest pancreatic cancer screening guidelines for high-risk patients from gastroenterologist Dr. Amitabh Chak.

New NCCN Guidelines Stress Genetic Testing For All Pancreatic Cancer Patients
Genetics impact your treatment for pancreatic cancer. Dr. Sapna Syngal discusses the recommendation of genetic testing for all pancreatic cancer patients.