Nurse Navigators Provide a Guide for the Pancreatic Cancer Journey

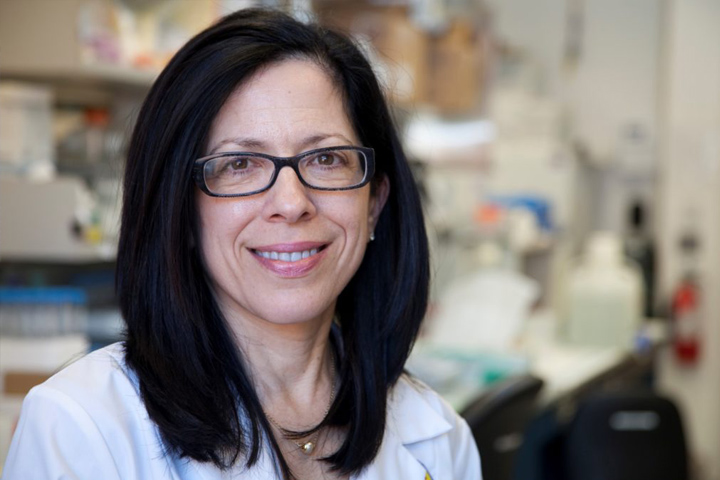
One of the first things pancreatic cancer patients notice about Patricia Gambino is that she asks a lot of questions.
As a gastrointestinal nurse navigator specializing in pancreatic cancer, it’s Gambino’s job to get to know pancreatic cancer patients and be a guide on their journey through treatment at the Penn Pancreatic Cancer Research Center, at the Perelman School of Medicine, University of Pennsylvania, in Philadelphia. She is a care coordinator, an educator, and an advocate. She provides support not only for patients and their families, but also to doctors and other members of the interdisciplinary team caring for the pancreatic cancer patient.
Gambino, a registered nurse with a Master of Science in Nursing, is one of a growing number of nurse navigators employed by hospitals and treatment centers around the country to help cancer patients navigate the increasingly complex, interdisciplinary care network they face after diagnosis. “Treating cancer is complicated. Treatment options are exploding. From precision surgery to targeted therapies, immunotherapies, and various modalities for radiation, it can be confusing and overwhelming for a patient,” she says. “I’m a very seasoned nurse who really understands GI cancers. I can triage the situation and know what the patient needs.”
Getting Started with a Nurse Navigator
To do that, Gambino asks questions. First, she gets to know her patient’s medical history. Does the patient have adenocarcinoma, like Patrick Swayze and most other pancreatic cancer patients, or a neuroendocrine tumor, like Steve Jobs, Aretha Franklin, or Ruth Bader Ginsburg? Depending on the type of tumor, and its genetic mutations, there may be different therapies available.
Gambino always encourages patients to enroll in a clinical trial, if there is one available that they are eligible for. A patient’s medical history will also factor in to the proposed treatment. For instance, if the patient had been perfectly healthy prior to his or her pancreas cancer diagnosis, he or she may be able to tolerate a much more aggressive treatment than a patient in poor health when diagnosed. In fact, there are times when Gambino discourages patients from traveling a distance to come to the cancer center if their health is so poor that they can barely get out of bed. When patients come to the cancer center for an evaluation, she helps to streamline their visit by coordinating as many consults as possible for the same day.
She also asks about their personal needs and wishes. “A lot of times it’s a matter of letting the patients tell you what they want. They may feel they cannot handle any more chemo, but they want to ensure they’ve left no stone unturned. They may be afraid of disappointing family by not pursuing other treatments,” Gambino says. “You really have to listen.”
Another aspect of treatment that she monitors is cost to the patient. Cancer care can be expensive, and treating pancreatic cancer often involves a multidisciplinary team of doctors: the medical oncologist, radiation oncologist, and surgeon. Gambino explains that if the patient’s insurance policy requires that they pay $40/consult, and they are to see three doctors in one day, that’s $120 that they weren’t counting on spending. Additionally, if their insurance policy dictates that they pay a 10 percent co-insurance for outpatient procedures, a $5,000 MRI will leave them with a $500 bill to pay, which can be tough for seniors or families with limited financial resources.
In Her Own Words
Every day I receive calls from patients who have just been told they have pancreatic cancer. They are overwhelmed with the news and don’t know where to begin. I listen to them to determine what are their most pressing needs. Are they experiencing any symptoms such as pain, inability to eat, jaundice (a yellowing of the eyes and skin)? It is the mission of the pancreatic interdisciplinary team to treat a new diagnosis of pancreatic cancer as a medical emergency, similar to a patient having a heart attack. It is imperative that the patient be seen by the right doctor at the right time in the trajectory of their cancer treatment.
For instance, if the patient is experiencing jaundice (because the cancer is blocking one of their bile ducts) we need to get them in to see a gastroenterologist for stenting. If the patient has not had a tissue diagnosis yet, then they may need to see a doctor who can biopsy the tumor for tissue confirmation, prior to seeing the medical oncologist.
Insurance coverage is also important to consider when a patient is considering treatment options. If a patient has insurance that is not accepted within our health system, I help them find a treatment center that treats a high volume of pancreas cancer and that is within network. This is important because there are many options today to treat pancreas cancer, such as precision surgery, targeted therapies, immunotherapies, and various modalities for radiation. Such treatments are not cheap; therefore, it is imperative that the patient seek a facility where their insurance is accepted. And of course, especially in the treatment of pancreas cancer, it is important to consider enrollment in a clinical trial.
Taking Back Control
But the biggest gift Gambino can give patients is the feeling that they can regain control over their illness. “Their whole life has been ripped apart and they are panic-stricken. They feel so out of control; it’s truly an out-of-body experience. I give them things that they can do so that they don’t feel so helpless,” Gambino says.
This includes advice about steps they can take to make sure their nutrition is up to par—an important goal to optimize treatment. She also arms them with information about the disease, the latest research developments, and available support networks, including connections to long-term pancreatic cancer survivors whose honest accounts about their treatment and recovery have helped many face the journey ahead. “They want to know the truth,” Gambino says. “It’s a difficult journey, and they want to enter it with eyes wide open.”
The benefits of Gambino’s services also extend to her colleagues. “It can be emotionally draining for the doctors and nurses treating patients with pancreatic cancer, as the care is very complicated.” She tries to coordinate the entire team (such as social workers, dieticians, financial counselors, physical therapists), so the patient is optimally supported.
Integral Part of the Team
Gambino is part of a larger clinical research team that involves physicians, scientists, radiologists, dieticians, social workers, financial counselors, and integrative service specialists who can offer complementary therapies such as Reiki, yoga, or massage. She attends clinical case discussions and is constantly reading the latest research to stay current about advances in the field.
In Her Own Words
As a nurse navigator, I must keep my knowledge current. It is important that I enroll in in-services that update me with current treatment of pancreas cancer. As a member of the interdisciplinary team, I attend tumor boards, where patient care is discussed.
It is also important that the nurse navigator be involved in community organizations that help support and guide pancreatic cancer patients. The overall goal of the nurse navigator is to support both the patient and the family throughout the trajectory of the cancer journey, providing education, advocacy, and access to leading-edge treatment.
“It’s important not to give false hope, but I let them know that there are options,” Gambino says. “I hate it when doctors tell patients, ‘Get your affairs in order and take a nice vacation.’ That statement gives patients no hope. There’s so much going on with pancreatic cancer treatment today and there is hope. It’s an exciting time.”
Juggling at least 50 cases at a time, with at least three new calls a day, the job definitely keeps Gambino busy. But she loves it. “I feel like it’s the culmination of my career,” Gambino says. “I spent 30 years as an oncology nurse in different positions within our health system. In the nurse navigator role, I can apply all I’ve learned from those various positions to caring for pancreatic cancer patients. I honestly feel privileged to be able to be with patients and their families during their difficult times.”