Focus on Nutrition with The National Pancreas Foundation

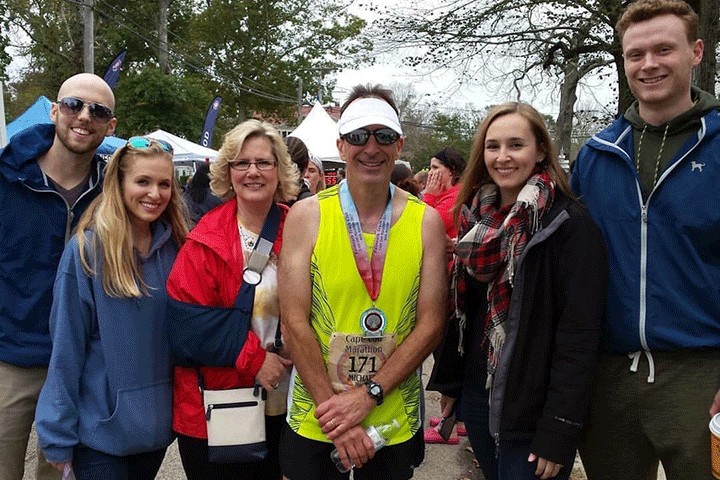
Clockwise from left: Patter Birsic, Sally Sampson, Dr. Anna Evans Phillips, Jane Holt
Every type of pancreas disease from pancreatitis to pancreatic cancer comes with challenges related to eating, digestion, and absorbing nutrients.
That’s one reason why The National Pancreas Foundation (NPF) focuses their efforts on educating patients, caregivers, and healthcare professionals about nutrition.
“Nutrition is so important for people with pancreas disease, and yet, many patients struggle to meet their nutrient needs,” says Anna Evans Phillips, M.D., M.S., Assistant Professor of Medicine at University of Pittsburgh Medical Center, Pennsylvania. To help alleviate those challenges, the NPF has designed a bevy of tools to educate patients, caregivers, and health professionals about best practices for navigating pancreas disease.
National Pancreas Foundation Basics
Founded in 1997, the NPF is the only foundation dedicated to patients who are suffering from all forms of pancreas disease, including pediatric pancreatitis, acute pancreatitis, chronic pancreatitis, and, of course, pancreatic cancer.
“The Foundation operates through donations of time, energy, and financial support from organizations and individuals who have been touched by pancreas disease,” says Jane Holt, co-founder of NPF and chronic pancreatitis patient. “With those resources, the NPF has given more than $5 million to fund over 130 groundbreaking research projects.”
From the beginning, educating patients, caregivers, and healthcare professionals about nutrition has been a key part of the NPF’s mission. Founded on the premise that food, and pain, sets pancreas patients apart from friends and family, former NPF Board Member Sally Sampson developed a cookbook to help ensure pancreas patients wouldn’t be singled out due to dietary restrictions.
Sally’s daughter, Lauren, was born with pancreatitis, so she was intimately aware of the challenges inherent in preparing meals that Lauren could eat but that also appealed to the entire family. Sally channeled her passion for food and recipe development into creating low-fat, high-flavor recipes that pancreas patients can enjoy alongside their families and loved ones. The end result: The NPF Cookbook. [Click on the link to download the cookbook or order a printed copy.]
“For patients with pancreas disease, every person’s nutritional situation is unique. The NPF’s pancreas disease cookbook is a helpful resource for patients to tailor recipes that meet their personal needs,” says Phillips. “I also recommend that patients talk to a pancreatologist or a registered dietitian about how to best meet their unique nutritional needs.”
The Role of Nutrition
If you or someone you love has pancreatic cancer, you know that nourishing the body through food is a top priority. Studies show that a healthful diet can help patients circumvent the weight loss and appetite changes that often accompany pancreatic cancer and its treatment, while also improving health outcomes. Yet, patients face myriad obstacles to attaining optimal nutrition, both during treatment and beyond.
“Since one of the roles of the pancreas is to help the body convert food into fuel, it makes sense that pancreatic cancer patients may struggle to properly digest food,” says NPF co-founder Patter Birsic. “There are many times when it’s difficult to eat at all.”
The NPF cookbook is a great starting point. From there, the following eat-right strategies can help ensure you meet your nutrient needs throughout treatment and beyond:
- Eat small meals. Pancreatic cancer can interfere with your body’s ability to digest food. To minimize the hit, eat small, easy-to-digest meals throughout the day. Struggling with poor appetite? Set an alarm to eat protein-rich foods every three to four hours.
- Amp up the protein. Protein helps your body build and repair cells, so it’s critical to get sufficient protein when you have pancreas disease. Lean protein sources, such as beans, poultry, fish, eggs, and tofu, are the easiest to digest. Aim to include one or more protein-rich foods in every meal and snack.
- Watch the fat. How much fat you should eat depends on a variety of factors, but in general, people with pancreatic cancer should aim for a low-fat diet. To aid digestion, spread fat consumption across meals, rather than concentrated into one sitting.
- Eat a rainbow of fruits and vegetables. The rich color in fruits and vegetables like tomatoes, eggplant, berries, and leafy greens represent different disease-fighting chemicals. To maximize the impact of these high-powered foods, aim to get at least five servings of fruits and vegetables daily.
- Limit sugar and fat. Pancreatic cancer can make it difficult for the body to digest sugar and fats. To help out your ailing pancreas, avoid high-sugar, high-fat foods like ice cream, cookies, cake, and fried foods, and focus instead on foods that have high nutritional value.
- Stay hydrated. Dehydration can cause inflammation in the pancreas, so it’s important to drink plenty of fluids. A good rule of thumb: Aim to drink half of your weight in ounces daily. So, if you weigh 150 pounds, try to drink 75 ounces of water daily.
- Keep a food diary. Consider starting a daily journal where you not only record what you eat and when, but also how you feel. It’s also a good idea to document your bowel movements, including when you go and notes about color, consistency, and form. This kind of detailed information can help guide treatment decisions.
- Get moving. Exercise not only helps enhance your mood and stimulates appetite, but it’s also associated with better treatment outcomes. In fact, research suggests that exercising before, during, and after treatment has dramatic beneficial effects for pancreatic cancer patients.
It’s important to note that pancreatic cancer and its treatments can cause changes in bowel habits ranging from diarrhea and gas to constipation and bloating. “If you experience changes in your bowel habits, or notice greasy stools, talk to your healthcare provider,” says Phillips. “You may need to take supplemental pancreatic enzymes with meals to help with digestion.”