Practical Tips For Patients In Treatment
When you’re about to embark on your first course of treatment for pancreatic cancer, the last thing you are thinking about is maintaining your regular medical care for things like your eyes or teeth.
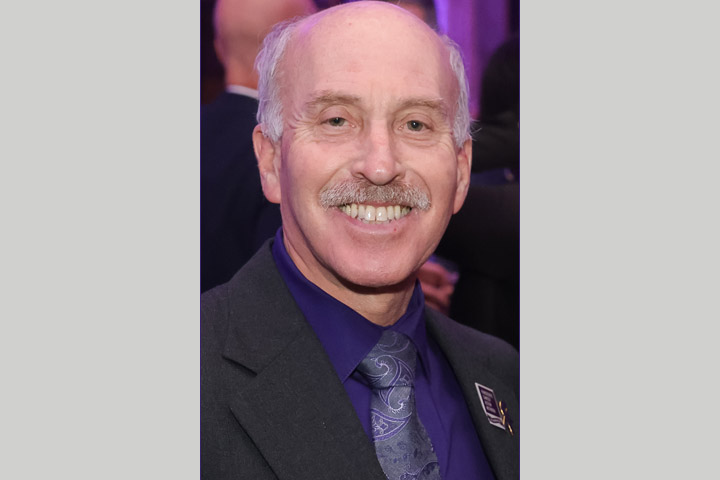
But as 12-year pancreatic cancer survivor Steven Merlin can attest, it pays to be proactive and diligent. “I survived the worst case scenario cancer by keeping a cool head and positive attitude, focusing on what I could do and what was available to me in helping to better tolerate and complete treatment to achieve a better outcome,” he says. “You need to focus on what is in your control while your medical team focuses on what you can’t control.” Merlin underwent 27 months of continuous chemotherapy after being diagnosed with pancreatic cancer in 2012 at the age of 55.
Despite the often harsh regimens of Gemzar, then FOLFIRINOX and a trial PARP inhibitor therapy, Merlin focused on having the best patient experience possible, and took a proactive approach to improving his quality of life during treatment
The career biomedical technologist and researcher is now often found in medical centers serving a different purpose: spending time with patients as they undergo infusions, giving support and advice to them and their caregivers. Merlin is also very active on online sites as a contributor and moderator, and on several cancer nonprofit boards as a patient advocate and consultant. As part of his advocacy, he has put together some top tips for current patients.
Dental Care Is Top of the List
First and foremost on Merlin’s list is dental care. “Do not postpone dental issues while undergoing treatment. Ignoring dental procedures could lead to bone and tooth loss, and progress to bacterial endocarditis, which can be life-threatening,” he warns.
Prior to starting chemo, have a thorough exam and cleaning. Then keep up with care by brushing or rinsing your mouth after each meal, and flossing daily and using interdental brushes. It is best to avoid extensive dental procedures while you are undergoing chemotherapy, but even then do not avoid a visit to the dentist if necessary—dentists and hygienists are trained to deal with immunocompromised patients.
Merlin speaks from experience. He learned all about dry mouth, sores, and “chemotherapy caries”—tooth decay brought on by changes in the bacteria in the mouth—during his long course of treatment. There are many affordable products you can use for mouth sores, sensitive teeth, receding gums, and dry mouth, including disks that promote overnight salivation and prevent too much bacterial buildup. In many cases, a simple $10 fix can save you a lot of agony and cost down the line, Merlin explains.
The Ins and Outs of Diet Issues
When it comes to diet, patients face issues with how food tastes and problems with digestion. Merlin has tips for both.
Chemotherapy can change the way food tastes, or introduce sensitivity in your mouth and throat, presenting new challenges when eating. If food tastes bland or unappetizing, try spicing things up with seasonings you may have avoided in the past. Merlin notes that he developed a taste for scrambled eggs drenched in Tabasco sauce.
If you’re losing weight during or after treatment, you may need enzyme supplements like pancrelipase to help digest your meals. The best-known brand names include Creon®, Pancreaze®, and Zenpep®. Merlin was six years into his treatment and recovery before realizing that he needed enzymes. He now urges others to ask their doctor for a prescription. If the doctor is wary, request a fecal elastase test, which measures digestive enzymes in your stool.
To figure out the ideal dose of pancreatic enzymes you need based on meal ingredients and quantities, there’s a handy online dosing calculator at digestthis.ca. And if you have difficulty swallowing enzyme capsules, try mixing them with room temperature apple sauce, followed by water.
For other digestive issues, diarrhea relief medications may help. The brand Imodium is the go-to solution, but it may not work for everyone, so don’t be afraid to ask about alternatives. The same is true for nausea and vomiting. There are three different pathways that trigger these symptoms, and different medications to target each of them, Merlin notes.
“Be proactive and start taking anti-nausea meds early to prevent any discomfort before it happens,” he adds. “I went through two years of intensive chemo and never once was nauseous or vomited.”
Preventing Peripheral Neuropathy
One of the challenges patients often encounter when undergoing the FOLFIRINOX chemo regimen is peripheral neuropathy, or tingling and numbness in the hands and feet due to nerve damage.
There are a few medications that can be prescribed to treat chemo-induced peripheral neuropathy, including duloxetine (Cymbalta®), gabapentin (Neurontin®) and pregabalin (Lyrica®). It usually takes at least a week before you feel the effects.
There are also other options, including cold therapy, in which gloves and slippers with cold packs are used during the 90-minute infusion of oxaliplatin to prevent neuropathy. It makes the drug less toxic to the peripheral nerves, while still remaining toxic to the cancer cells.
If you and your medical team are willing to lengthen the infusion time of the oxaliplatin, this could provide yet another option for relieving neuropathy. In consultation with his doctors, Merlin decided to undergo six cycles of full FOLFIRINOX therapy, followed by six ‘resting’ cycles with two of the four chemotherapy drugs removed. He repeated this several times, for 46 total cycles (24 at full dose—twice the 12-cycle standard-of-care).
Do Your Homework
Merlin was able to take control of his treatment because he became deeply integrated into his care team. He did his homework and turned up to appointments prepared to ask questions.
“Don’t just passively listen to what you are told, take an active role in your care and don’t be afraid to speak up,” he says. “Show the care team that you really want to survive. Demonstrate that you are serious and that you are going to put effort into your own treatment.”
Get to know everyone on the team, including members you might not have considered, such as the hematology/oncology pharmacists who prepare the medications for your infusions, he adds. They are great resources if you are considering taking supplements or modifying your treatment in any way. Making informed decisions about this is essential, since any other medications could have unintended consequences, such as changing the way your body metabolizes the chemo drugs, negating the effects of chemo or making the drugs more toxic, which could in turn harm critical organs like your liver or kidneys.
Stay Positive
When patients feel good, they are more likely to stick with their treatment and get the full benefit. Merlin is a big believer in managing quality of life issues, and speaks to oncologists and clinical trial teams often about incorporating patient quality of life measures into trial and treatment protocols.
He’s also a testament to the power of positive thinking and action. Throughout his treatment, he continued with moderate exercise and never missed a day of work. “If I was going out of this world, I was going to go out running, not crawling and whimpering,” he notes.
Merlin is now 12 years cancer free, and as close to cured as possible. He’s still on a PARP inhibitor, but no longer dreading the results of his blood tests and surveillance scans every six months.







