A Life-Changing Diagnosis: My PNET

- Stomach issues brought me to the doctor
- Family history led to PNET diagnosis
- Da Vinci® robotic surgery
- Pancreatic enzymes needed after
After months of constant stomach issues, awful cramps, nausea, and loss of bowel control, I sought the help of a local gastroenterologist in March 2023.
We live in a relatively small community in Fernandina Beach, Florida, which doesn’t have a wide variety of specialists or advanced technology. I visited the gastroenterologist several times that spring and the only thing I was told was to try the FODMAP diet, which eliminates certain foods to see if certain triggers for digestive problems can be identified.
Initial Diagnosis: My Diet?
Many patients may know of the FODMAP diet and like it, but it seemed to me a very antithetical diet given my symptoms. Or maybe it was another way for the specialist to say, “I don’t know what’s wrong with you.”
I researched my symptoms extensively because I wasn’t satisfied with the initial diagnosis and lack of treatment protocol. I met again with the specialist and mentioned that I had a cousin that had died at a relatively young age of pancreatic cancer and that several others in my family that suffered from pancreatitis. At last, a bell went off and she prescribed a CT scan.
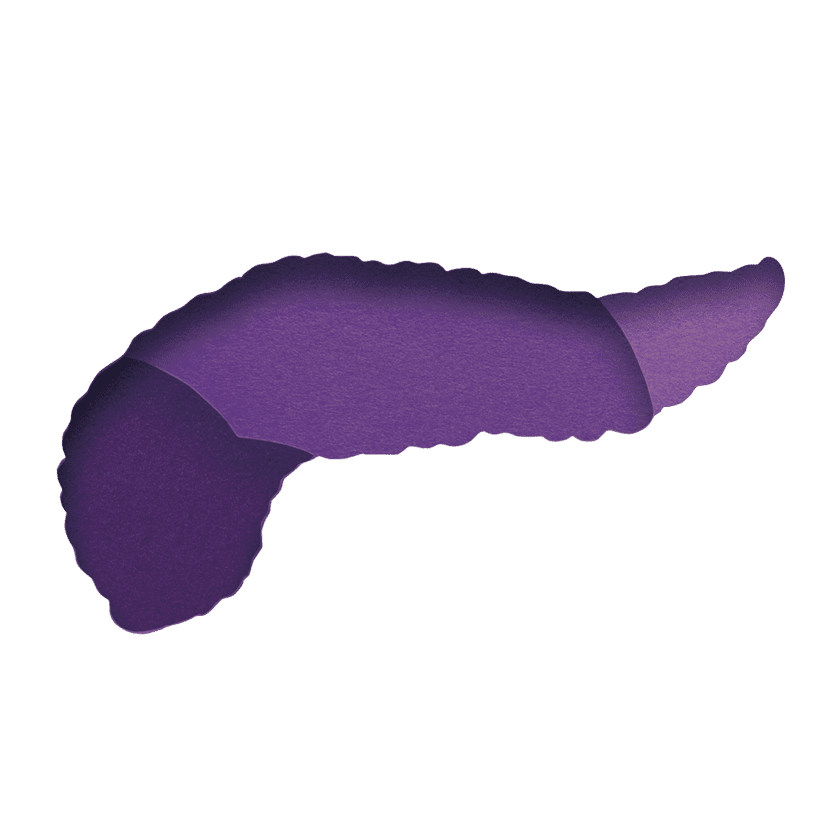
However, our city doesn’t have a CT scan facility, so I visited a specialist in Jacksonville instead. He performed the test and confirmed there was a small PNET (pancreatic neuroendocrine tumor) located in my pancreas. He urged me to have an endoscopic exam to be entirely sure, which I did.
PNET Confirmed
The endoscopy confirmed my PNET diagnosis, and the next recommendation was to have it surgically removed. Again, I did more research to understand exactly what kind of surgery was available to remove a PNET. I selected Dr. David Neimeyer, a surgeon at Baptist Health Hospital in Jacksonville, who planned a minimally invasive laparoscopic surgery with the da Vinci® robot.
Dr. Neimeyer indicated that he wouldn’t know what to expect of my tumor or the surgery’s outcome until he actually got in there to see it for himself. I decided to move forward even though there was still so much ambiguity. The tumor ended up being small and not entangled with many of the tricky blood vessels surrounding it. Thankfully, he was able to remove all or most of it with the robot.
A Positive Outcome
While the surgery itself took longer than we had expected, the outcome was very positive. I was on a beautiful surgical floor in a private room for only three days with wonderful caring people all around me. I had a follow-up appointment with the surgeon after that.
The complete recovery took about three months. I experienced discomfort and fatigue initially. My doctor prescribed CREON to help replace the pancreatic enzymes I had lost. As most survivors and patients with pancreatic cancer know, fatigue can be the enemy.
I later had a PET scan at Baptist MD Anderson Cancer Center in Jacksonville to ensure that all those pesky cancer cells did not migrate. So far, so good. I had another appointment with the oncologist, Dr. Robert Zaiden, at MD Anderson at the end of November 2023 and will continue to have them annually. So far, no extensive treatment protocols have been required.
One thing that helped me was a 12-week program called Livestrong, which is available for free at many YMCAs across the country. Survivors and/or patients can apply for the program with their doctor’s approval. They engage in activities that strengthen muscles through mild exercises and the ability to communicate with others about their specific issues and goals.
Do Your Research!
I can only suggest, if patients are symptomatic with the stomach issues I mentioned, please do your research on treatment protocols, qualified specialists and surgeons, and an understandable diagnosis. After 77 years, I’ve learned to question issues regarding my body and not to accept just one point of view or diagnosis. All of my research paid off and I am grateful for it.