Pancreatic Neuroendocrine Tumors (PNETs)
Learn the Basics
Steve Jobs and Aretha Franklin have more in common than being famous. Both also had the same rare form of pancreatic cancer, called pancreatic neuroendocrine tumors (PNETs). More recently, television host Maria Menounos received treatment for the same condition.
To learn more about living with PNETs, read our stories of survivors who have undergone different treatments. For more information about PNETs, read Living Longer with Pancreatic Neuroendocrine Tumors.
Although Rare, PNETs Have a Better Outlook
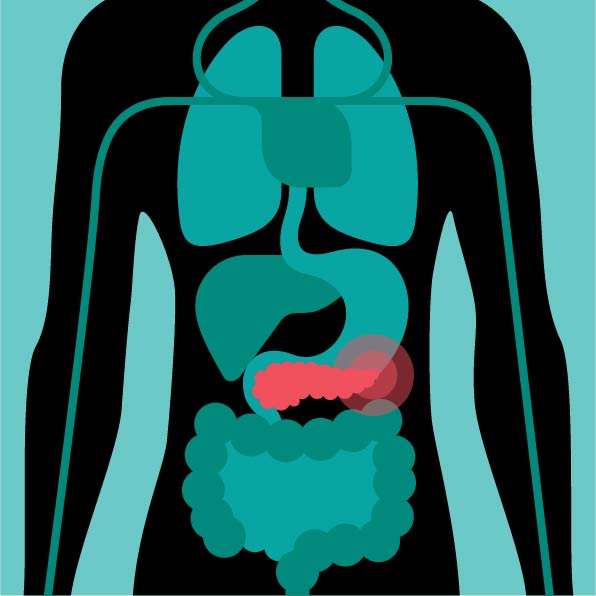
Pancreatic cancer generally falls into two different categories, exocrine or endocrine cancer. Exocrine, called pancreatic adenocarcinoma, is the most common form, which accounts for 90 percent of all pancreatic cancers. Patients with adenocarcinoma have a 13 percent five-year survival rate. PNETs, however, are endocrine cancers. While PNETs affect only five to 10 percent of all people with pancreatic cancer, the five-year survival rate is 53 percent; for patients with cancer that has not spread outside the pancreas, the survival rate increases to 95 percent
Different Types Cause Different Symptoms
PNETs form in special cells found inside the pancreas called islet cells, a type of neuroendocrine cell. These cells produce hormones that include insulin, glucagon, and somatostatin, which regulate blood sugar and other functions in the body.
PNETs grow slowly—often over the course of several years. Most patients rarely notice symptoms early on, particularly if they have a type of tumor that does not secrete hormones.
One unique feature of PNETs is their different symptoms. Like adenocarcinomas, PNETs can cause nausea, vomiting, abdominal pain, and weight loss. But there are different types of PNETs, and each stands out because of their unique signs and symptoms, which vary depending on the type of tumor
Insulinomas make excess insulin, which gets secreted into the bloodstream and can cause low blood sugar, with symptoms including sweating, anxiety, lightheadedness, and fainting.
Gastrinomas make excess gastrin, leading to more stomach acid, causing abdominal pain, nonhealing stomach ulcers, reflux, and weight loss.
VIPomas make excess vasoactive intestinal peptide, causing abdominal cramping, watery diarrhea, and facial flushing.
Glucagonomas make excess glucagon, raising blood sugar levels, and can cause diarrhea, excessive thirst or urination, and weight loss.
Somatostatinomas make excess somatostatin, which regulates other hormones, and result in diarrhea, weight loss, abdominal pain, and foul-smelling fatty stools.
PPomas make pancreatic polypeptide, which regulates endocrine and exocrine cells in the pancreas and cause belly pain and an enlarged liver.
The pancreas is not the only organ in the body that contains neuroendocrine cells. These cells can be found in the stomach, small bowel, adrenal glands, thyroid, lungs, and other organs. About 177,000 people living in the United States have some sort of neuroendocrine cancer. However, PNETs only come from the neuroendocrine cells in the pancreas.
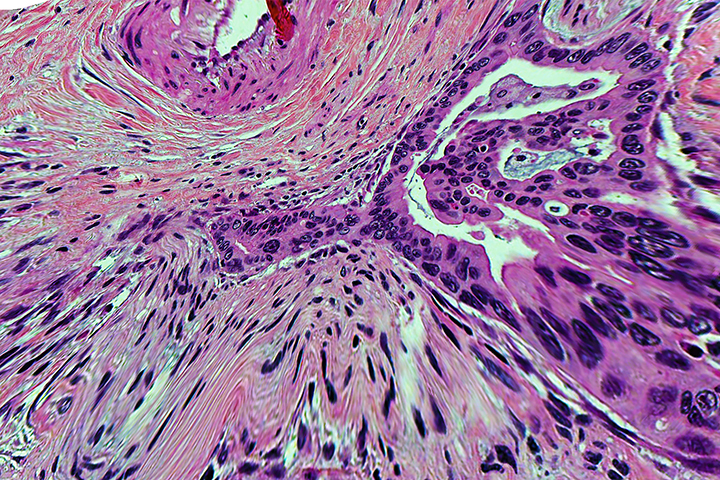
Tumor Grading
Doctors classify PNETs by how quickly they think the tumor will grow and spread. This classification system is by tumor grade, and PNETs fall into three different categories
Grade 1 PNETs have normal-looking cells that do not multiply quickly. This category is also known as well-differentiated or low-grade.
Grade 2 tumors, also known as moderately differentiated or intermediate-grade tumors, have traits between those seen in grade 1 and grade 3 tumors.
Grade 3, poorly differentiated or high-grade neuroendocrine tumors have cells that look extremely abnormal and reproduce faster.
Different Treatments
As with adenocarcinoma, treatment can involve surgery, ablation or embolization, drug therapy (including targeted therapy and chemotherapy), or radiation and possibly radioactive drugs.
Surgery for PNETs is based on the location of the tumor within the pancreas. A patient may have a distal pancreatectomy (tumor in the tail), Whipple procedure (in the head), a total pancreatectomy (removal of the entire pancreas), or more limited surgery that removes just the tumor.
Ablation or embolization are different ways to destroy tumors. Ablation uses different forms of extreme heat or cold to destroy tumors, while embolization blocks blood supply to tumors by using chemicals, radiation, or physical blockers.
Drug treatments vary depending on the type of PNET and how far it has spread.
- For patients with advanced PNETs, there are other drugs that can be used. Tumors with somatostatin receptors can be treated with octreotide or lanreotide, which can help with symptoms caused by the tumor as well as improve outcomes.
- Targeted drug therapies work on very specific parts of the cancer cells. Ones often used for PNET treatment include sunitinib, everolimus, cabozantinib, and belzutifan.
- Chemotherapy is used when the cancer is advanced, when other drugs have not been effective, and when the cancer is high grade. Many of these are the same drugs used to treat adenocarcinoma.
- Immunotherapy with pembrolizumab (Keytruda) is given to patients with certain tumor profiles, such as high microsatellite instability or a defect in the DNA mismatch gene repair.
Radiation therapy can include standard radiation treatment as well as radioactive drugs. There is a newer treatment called peptide receptor radionuclide therapy (PRRT), which works on PNETs that are positive for somatostatin receptors, and delivers a radioisotope to the cancer cells to kill them
Clinical trials are another option to consider for treatment. Our Trial Finder can select PNET trials to consider.