Decoding the Differences between At-Home and Medical Genetic Testing

For the last few years, at-home genetic tests have been all the rage, with advertising showing people eagerly learning their families’ supposed origins.
Genetic testing has become important to pancreatic cancer patients as well. According to updated guidelines from the National Comprehensive Cancer Network, all pancreatic cancer patients—and, in some cases, their immediate family members—should undergo genetic testing. Certain provinces in Canada, too, push for medical genetic testing for pancreatic cancer patients, though it’s not funded through the Ministry of Health.
Results of these genetic tests not only uncover whether you have a gene that played a supporting role in the development of your disease. Studies show that around 10 percent of pancreatic cancers have a strong inherited component. This information can be important to know, since certain genetic mutations can inform which treatment protocol will result in the best outcome.
Finding inherited genetic risk can also provide critical information for family members who are not ill, such as adult children, siblings, aunts, uncles, and cousins. Relatives can be tested to see if they too inherited the gene mutation. Those who did may benefit from special follow-up care, often starting at an earlier age. Being proactive could lead to life-saving interventions.
The testing also benefits the relatives who did not inherit the gene mutation. They do not need to have this more aggressive care and can be reassured they could not have passed this on to their children. Genetic testing information is important, when coupled with expert medical advice and targeted with the right care.
But in the age of information and easy access to commercial genetic tests—it is a multi-billion-dollar industry—do you really need to see a doctor or genetic counselor to test your DNA? In a word, “yes.”
Different Types of Tests
At-Home Genetic Tests: Also called “direct-to-consumer genetic tests,” at-home genetic tests are marketed directly to patients through print, television, and internet advertisements. Customers purchase these tests online or in a store. Then, they collect their own DNA (usually by spitting into a vial) and ship the sample to the company. Six to 10 weeks later they receive results directly from the company through a secure website or via written report. Some genetic testing companies, such as Color and Helix, have medical grade tests that are also available direct to the consumer.
Although the “direct-to-consumer” option may provide standard boilerplate information about results, it does not include expert personal advice of what the results mean for you or your family members.
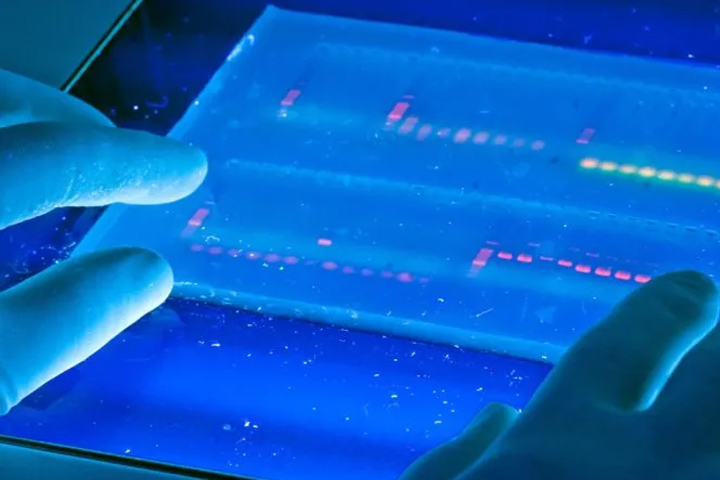
Medical Grade Genetic Tests: With medical grade genetic tests, a genetic counselor or physician orders the test, collects the DNA sample, interprets the results, and shares the results with patients.
Many, if not most, academic medical centers use commercial genetic testing labs, as opposed to in-house labs. The commercial labs have automated some parts of an extremely complex process, with the appropriately trained professionals at the helm.
What is the difference between the testing you see advertised and what you would get through a genetic specialist? Here’s how the two options compare:
At-Home Genetic Testing
Cost: Prices range from $99 to $1,000 or more, depending on the test.
Access: Good. Anyone with internet access—or the ability to pick up a 23andMe kit at a big box store—can easily purchase commercial genetic testing kits.
Accuracy: Limited. At-home tests from companies like 23andMe do single-nucleotide polymorphisms, or SNPs (pronounced snips). While SNP testing uncovers variations at specific sites of the genome, those variations are like reading one sentence out of a 550-page novel. “The additional risk you might have from a SNP may be miniscule,” says Jill Stopfer, M.S., L.G.C., associate director of genetic counseling at Dana-Farber Cancer Institute in Boston.
Even more concerning, if you take the same sample to four different commercial labs, you may receive conflicting results. This doesn’t mean that one lab got it right and the others got it wrong. Each company’s test may use a differing set of SNPs and use different algorithms to determine cancer risks. These types of genetic tests don’t provide scientists with enough information to really assess risk.
In addition, medical assessments may not be comprehensive. Take 23andMe, for example, which was recently approved by the FDA to look at three specific mutations in the BRCA1/2 genes. “Those three mutations only apply to the Ashkenazi Jewish population—less than 10 percent of people of other ethnicities carry these variants,” says Heather Hampel, M.S., L.G.C., cancer genetic counselor and associate director of the Division of Human Genetics at The Ohio State University Comprehensive Cancer Center (Columbus, Ohio). “Even if you don’t have one of those variants, you could have one of the thousands of variants not included in the test that put you at higher risk.” So, the results you’re getting can be both misleading and falsely reassuring.
Privacy: Poor. Many direct-to-consumer genetic tests aren’t completely transparent about privacy concerns, and when they are, they say your data may be used for research and other purposes. Some companies keep genetic test results indefinitely.
Actionable information: Poor. Since SNP-based at-home tests are not comprehensive, meaning they don’t look at all of your DNA, most of the time you won’t get actionable information. The company will provide you with interpretation based on the SNP results. And you can send your results for further interpretation to third-party companies with poor track records. As Stopfer explains, published studies have shown that in about 40 percent of cases, these interpretations are rife with errors.
The bottom line: With certain types of at-home genetic testing, there’s a chance you’ll receive false information that will lead you to unnecessary, costly, and potentially harmful testing—or worse, you’ll gain a false sense of security that pancreatic or other cancers are not in your future.
Medical Genetic Testing
Cost: Minimal. If you’re testing because an immediate family member has pancreatic cancer and has been found to have a mutation in a cancer risk gene, your insurance will likely cover the cost for both the test and guideline-recommended screening that results from it. Even when insurance doesn’t kick in, the cost for basic medical genetic testing is under $300. The laboratories also provide generous support to defray the cost of testing for those with limited income.
Access: Good. The National Society of Genetic Counselors has a list of providers on their site who provide services both face-to-face and through cyberspace. True, you need an order by a medical professional to get medical grade genetic testing. But that actually works out in your favor. “You want those results in your medical record so your doctor can do the appropriate surveillance and catch the disease early,” says Hampel.
Accuracy: Good. With medical grade genetic testing, those with professional training in genetics can help determine the appropriate test. “These tests look at multiple genes at once, so a panel can include a varying number of genes,” says Stopfer. “In either case, the goal is to thoroughly examine an appropriate combination of genes, and which may be chosen is based on a person’s personal and family history of cancer.”
Privacy: Fair. Any health professionals (and insurers) who are managing your care can access your genetic testing information. Their ability to provide the highest quality care depends on having those results. However, a federal law prohibits employers and health insurance companies from discriminating against most individuals based on the results of genetic testing.
Actionable information: When you do medical genetic testing, specially trained genetic counselors interpret the results for you. There’s no wondering what your results mean or whether you need special screening. Instead, your doctor can assess your level of disease risk and offer you the latest and greatest screening protocols as appropriate. A bonus: “With the documentation of genetic risk, you meet national guidelines for coverage of appropriate follow-up screening tests, which should be covered by insurance,” says Stopfer.
The bottom line: Knowing your true genetic risk, which you can only get through medical grade genetic tests, may play an important role in which treatment protocol your oncologist selects. “We know, for example, that patients with a BRCA mutation respond well to PARP inhibitors,” says Hampel.
For family members whose genetic test results indicate they have an increased risk of pancreatic cancer, doctors may recommend annual imaging of the pancreas with magnetic resonance imaging, an endoscopic ultrasound where doctors thread a thin tube down your throat and into the bottom of your stomach to capture detailed ultrasound images of your pancreas, or a combination of both. “The hope is that we may one day be able to stop pancreatic cancer in its tracks,” says Hampel.
Trials for Genetic Testing
There are a number of efforts underway to promote genetic testing among the pancreatic cancer community and their family members. The GENERATE study (GENetic Education, Risk Assessment, and TEsting), for example, aims to enroll 1,000 participants to improve genetic testing and cancer prevention among family members of pancreatic cancer patients with inherited mutations. The study will also explore whether different approaches to genetic education increase the rate of genetic testing for these family members. Participants can work with genetic counselors to understand the testing process, and if tested, what the results mean.
At Columbia University, the Muzzi Mirza Pancreatic Cancer Prevention & Genetics Program focuses on genetic testing as part of an effort toward early detection of pancreatic cancer. Around 130 new patients visit the Columbia University center for genetic testing each year, and hundreds more are monitored through regular screenings and preventive treatment. The goal, of course, is to detect pancreatic cancer early so doctors can stop it from progressing.
There are also tumor registries, which collect information about families with more than one member who has been diagnosed with pancreatic cancer. Nearly 5,000 families have enrolled so far. Participation involves the completion of a health history questionnaire and, in some cases, a DNA sample. The data is entered into a computer program that creates a family tree, and helps researchers better understand how and why pancreatic cancer clusters in some families.
Have a deceased first-degree relative with pancreatic cancer? Many institutions have biorepositories with banked DNA from deceased patients. Families can perform medical genetic testing on that stored DNA to determine whether the patient’s pancreatic cancer was genetically linked. The sticker price for most of these tests: only $250.