At the Table: Advocating For Yourself
Although pancreatic cancer treatment can be overwhelming, advocating for yourself can be very helpful for you and your oncologist.
Don’t be afraid to ask questions when you don’t understand something. You can make your wishes known and get the best treatment at the same time. In this Round Table, pancreatic cancer patients and survivors discuss the different ways they advocated for themselves, what they learned, and what they might do differently.
Were You a Good Self-Advocate?
Doris Bowdoin: I knew to be diligent in my efforts to find the right person to treat me. I researched on the internet, but I also sought out recommendations. I got a referral from a renowned ovarian cancer doctor previously used by a family member, who sent me to a doctor at University of Alabama at Birmingham, a research institution where the doctors are up on the latest treatment. I was willing to travel there from my home in Florida.
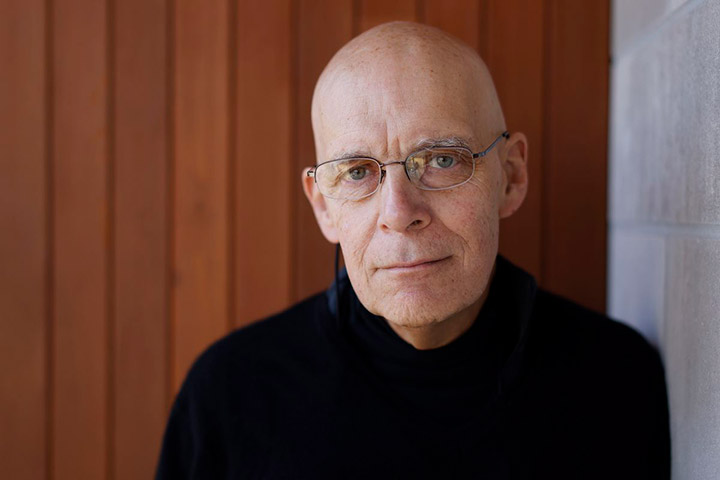
Robert Weker: I think I was a good self-advocate in some areas and not so good in others. For example, I was a strong advocate on choosing my medical team and pursuing treatment at a multidisciplinary clinic. We changed my oncologist early in the process as my original oncologist/his team was just not a good fit. Best decision I made!
Sandy Robis: As a two-time cancer survivor (breast 12 years ago and pancreatic 2.5 years ago) and having lost my mom to pancreatic cancer, advocating during care is not new to me. It is critical to the quality of care we receive as well as the quality of life we live. It is paramount that we educate ourselves on our disease. Knowledge is power and enables more powerful advocacy.
Eric Borden: If I wasn’t a good self-advocate I might not be here today. Never take anyone’s word as gospel. It is important to learn everything you can in order to make your own educated and rational decisions.
What Did You Do That Helped Direct Your Treatment?
Eric: I was told to wait one year and come back for another scan. Instead, I asked questions and educated myself, and decided to seek further treatment and opinions. If I had waited, my cancer would have spread and might not have been treatable.
Randall Swan: I spent countless hours researching surgeons, clinical trials, and different treatment. I even solicited help from a friend who is a chemical engineer to help sift through the information.
Robert: I wanted to partner with my medical team. I was struggling with pain management after my Whipple and different doctors were telling me to do different things including, seeing an additional doctor. I finally emphasized that I’m the least qualified to make this decision and did not need another doctor added to my already large team. Bottom line, my oncologist took full ownership and coordinated the information I was getting.
I was a strong advocate in my treatment. I coordinated with my oncologist to let me use oral chemotherapy agents instead of an infusion pump, in conjunction with proton beam radiation.
And finally, I decided I wanted to participate in a clinical trial. I had an advantage in finding a good clinical trial, given that I worked for a pharmaceutical company and my colleagues were able to help me find a good trial, close to home in a very efficient manner.
Sandy: Self-advocacy is literally a daily activity for me. From the very beginning, I understood the severity of this disease and knew that time was of the essence. I would not tolerate delays or cancellations of any sort even during COVID. I experienced suspicious symptoms on a Sunday. By the following Saturday I had seen my primary care doctor, had lab work, an ultrasound, CT scan, made contact with a surgeon, and scheduled an ERCP for the next Monday to put in a stent to relieve my jaundice. It was two weeks before Christmas and the surgeon recommended waiting until early in January to remove the mass on my pancreas, but I insisted on getting it done before Christmas (2018). And when I had a recurrence in 2020 I advocated for a second opinion at a major pancreatic cancer center to confirm the new chemo regime.
I also had to advocate for genetic testing (especially given all the cancer in my family) and molecular profiling. With help from the Pancreatic Cancer Action Network (PanCAN) and my local oncologist we were able to identify clinical trials they felt I may be eligible for.
Doris: I was on a feeding tube for a long time, and after it was removed I really concentrated on nutrition. I also made myself get up and move as much as possible. Lastly, I surrounded myself with a great core of family and friends. Love and laughter are so important and help you to stay positive!
What Would You Do Differently Knowing What You Know Now?
Robert: It would have been helpful to have a “playbook” in place for new patients and caregivers. We needed more information about what we should be concerned about and how to address these issues, both short-term actions and also long-term issues that need to be addressed early on. Some examples include legal issues such as work and the type of leave to take. Others are related to treatment, including how to wean off of OxyContin after a Whipple and how to minimize the impact of soft nails/neuropathy.
Randall: I would have provided more support for my wife, who was my caregiver.
Sandy: Pancreatic cancer is a very challenging cancer to diagnose and treat and time is not on our side, so moving quickly is imperative. Treatments vary by surgeon, medical oncologist, radiologist, medical facility, province/state, country, type of healthcare system, insurance coverage. This puts even more emphasis on educating yourself and self-advocating based on all you learn and can benefit from. And people should not shy away from getting second and third opinions throughout their journey.
Everyone and every facility talks about “patient-centric care and empowerment” but at the end of the day the buck starts and ends with us so you have to make your voice heard. I literally had to play quarterback and become Tom Brady to effectively manage and direct the vast team of specialists needed to manage my care.
In terms of doing something earlier, perhaps get the genomic testing done sooner so targeted treatments and clinical trials can be identified more quickly.
Doris: Stay with your doctor no matter the distance. I had several complications after my surgery and went to my local doctor or hospital rather than make the trip back to UAB. This caused me to be in a very weak condition by the time I did decide to get back to UAB.
Also, I would have loved to have someone to talk to or converse with during my struggle.
Eric: I wouldn’t do a thing differently. I’m here, to prove I was right! I’m certainly glad I listened to myself.