Tonsil Cancer Follow-up Finds Pancreatic Cancer
- Tonsillar cancer follow-up leads to discovery of a pancreatic tumor
- Distal pancreatectomy and splenectomy
- A second opinion regarding follow-up chemotherapy
In 2011, when I was in my early 70s, I noticed a slight swelling in my neck that my wife and I thought was due to sinus drainage.
After a few months I finally went to have it checked, and although the ENT doctor thought the same, he suggested a needle biopsy of my tonsil to be safe. I was surprised . . . no, shocked . . . when the pathologist came back and told me, “You have a squamous cell carcinoma.” In my disbelief, which I assume is common, I merely said, “You must be mistaken, I can’t have cancer!” I called my wife to tell her the bad news. After we both got over the shock, we went back to the ENT doctor to find out what to do. He recommended surgery and subsequent chemotherapy and radiation. I was scheduled for surgery the following week and was advised by Trey Fyfe, M.D., a friend who is also an ENT doctor, to ask for a consult with the surgeon prior to the surgery, to determine just what would be done, as there were different procedures available. When I asked for that, I was told that the surgeon was too busy to see me prior to the surgery. Since I did not care for the surgeon and found the ENT doctor unpleasant, I canceled my surgery and went to my friend for the procedure. It was successful, but he advised me to have the chemotherapy and radiation just to be safe, so I returned to Baylor Scott & White Medical Center in Temple, Texas, the original hospital I went to, for both. After seven weeks of daily radiation treatments wearing a “Prisoner of Zenda” mask to hold my head in place, and chemotherapy treatments, I was told that all should be good. I put those torturous weeks behind me.
A Surprise on Follow-up
In February of 2012 I went in for a PET scan, as a follow-up to the above, to ensure that all was well. My wife and I met with the head of radiation oncology at the hospital, and, in another unforgettable moment, he informed us that my tonsillar cancer had resolved, but . . . the scan had found a tumor on my pancreas. He said it was on the body of the pancreas and he led us to believe that I had only a short time left. I needed surgery, chemotherapy, and radiation again if I wanted a chance to go beyond that.
We wanted a second opinion, and another friend of mine, Shannon Cox, M.D., is a radiation oncologist, so I contacted him and asked him to look at the films and to meet with us. He contradicted the original report, saying that the tumor was on the tail of the pancreas, and not on the body, and that a distal pancreatectomy would take care of it and that I would be fine after that. It goes without saying that we were ecstatic about the news, and I scheduled the surgery at Baylor Scott & White Medical Center, due to its proximity to our home.
The surgery, which was deemed a success, included a splenectomy. During the recovery period I lost 30 pounds and walked around with a drainage port/bag for a few weeks, but eventually all returned to “normal.” After I recovered, we met with the original chemotherapy doctor, who recommended another round of chemotherapy and probable radiation. My wife had researched the toxic effects of chemotherapy, and particularly after my earlier experience with both, we declined and again sought another opinion from an oncologist with another medical practice. His opinion, after viewing all the films and records, was that I would be all right without the chemotherapy and radiation and that he would follow me to ensure that that was the case. He referred to me as a “2 percenter,” saying that I was very fortunate that it was caught so early because “98 percent” of people with pancreatic cancer do not survive. He also added that, ironically, my original throat cancer probably helped save my life. If that cancer had not been found, and the subsequent PET scan had not been done, the pancreatic cancer would not have been discovered until it was too late.
Life After Treatment
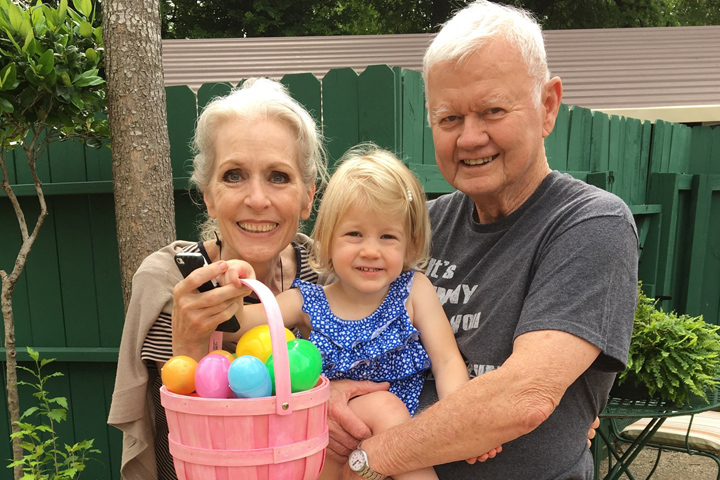
After a few years of follow-up scans and checkups I was dismissed from care for pancreatic cancer. I still have annual checkups that include labs for the cancer markers, and at 80 I continue to work full-time as a clinical psychologist on staff at a psychiatric hospital.
I have been a lifelong competitive tennis player and I was told that my physical conditioning contributed to my survival of everything above. I continue to play tennis and enjoy life, at least as much as anyone can during this COVID-19 craziness.
My wife Cynthia was a great patient advocate and challenged recommendations when she felt they were not appropriate for me, and she did this much better than I did for myself. If I could convey one thing to others it would be to trust their own instincts and not just always blindly rely on the advice that is given. Research options prior to making decisions and, above all, remember it is your life that is at stake, not anyone else’s.