An Update on Vitamin C and Cancer

Nearly six years ago, Lewis Cantley, Ph.D., Director of the Sandra and Edward Meyer Cancer Center, Weill Cornell Medicine, New York, and his team published findings in the journal Science showing high doses of vitamin C halted the growth of colon cancer tumors with KRAS or BRAF mutations.
That finding has moved into a phase II human trial of solid tumors such as lung, colon, and pancreatic cancers to confirm earlier results. The study’s estimated completion date is December 2021. The trial, supported by both Stand Up to Cancer and the American Association for Cancer Research (AACR), may prove the adage “Everything old is new again.” This is not vitamin C’s first foray into cancer. Nor is it the first attempt to rein in KRAS, a protein implicated in more than 90 percent of pancreatic cancers and considered “undruggable,” though researchers are making progress in targeting the gene. About 3 percent of pancreatic tumors have a mutation in another gene, called BRAF. About half of all colon cancers harbor a KRAS or BRAF mutation.
Making Sense of Vitamin C
In the 1970s, it was discovered that some properties of vitamin C may make it toxic to cancer cells. Early studies had promising results, but they were marred by controversy and found to be flawed. When researchers took up the mantle again, in randomized, controlled trials, it was found that vitamin C was of no benefit. However, those studies weren’t an apple-to-apple comparison to prior work. Nonetheless, vitamin C fell out of favor. Alternative medicine practitioners continued recommending high doses of vitamin C for cancer treatment.
Now, there’s a renewed interest in vitamin C among some of the nation’s top cancer researchers, spurred on by a better understanding of how it interacts with cancer cells. Plus, there is mounting evidence from early-stage trials that vitamin C can improve a patient’s quality of life—healthy tissues are spared the toxic effects of chemotherapy and cancer pain is minimized. Although scientists are quick to point out that vitamin C alone won’t cure cancer, it may boost the effectiveness of other treatments like chemotherapy or radiation therapy. “It all comes down to the mechanism of action, and the mechanism makes sense,” explains Cantley, who is considered one of the world’s leading experts in cancer metabolism. “What we have shown in a series of papers, in the context of cells with KRAS mutations, is these cells have an overexpressed glucose transporter. That’s why you can image these things with a PET scan. They’re taking up much more glucose.”
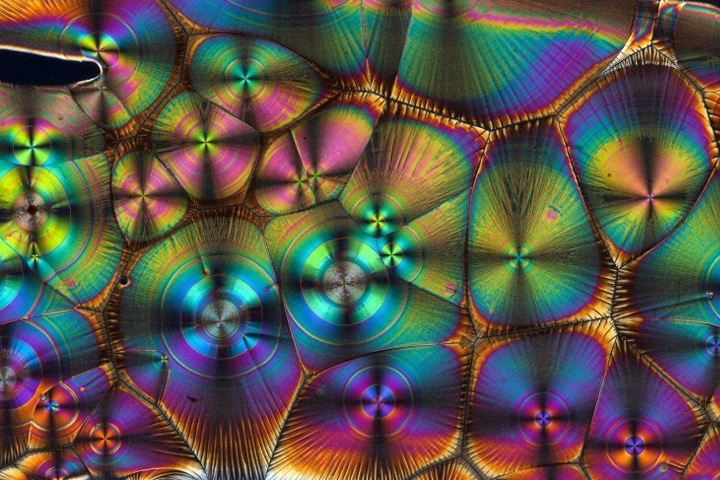
It’s this glucose transportation system that is key to vitamin C’s effects. The process is very complicated. But put simply, it seems that KRAS-mutated cells make an exorbitant amount of a protein called GLUT1. This protein’s job is to transport glucose across the cell membranes. In doing so, cancer cells get very high levels of the glucose they need to survive and thrive. GLUT1 also transports the oxidized form of vitamin C into the cells. This oxidized form of vitamin C is called dehydroascorbic acid (DHA).
When our cells are healthy, a very small amount of vitamin C is converted to DHA. But in the cancer-friendly microenvironment of a KRAS-mutated tumor, large amounts of vitamin C are converted to DHA. This oxidized form of vitamin C is bad news for cancer cells. “Once the DHA gets inside the cell it’s like a Trojan horse,” Cantley explains. That’s because there are antioxidants—molecules that try to prevent cell damage—inside the cancer cell that try to convert the DHA back to vitamin C to fight off the cell damage caused by the DHA. “What happens is the antioxidants get depleted and once that happens, the cancer cell dies from the DNA damage caused by oxidative stress,” he says. Tumors that have defects in genes that repair DNA, such as BRCA1 or BRCA2, are especially sensitive to being killed by vitamin C. Combining vitamin C with radiation to cause more DNA damage can enhance tumor killing.
About the Study
This is a multicenter, single arm, 3-cohort, open-label trial of high-dose vitamin C intravenous infusion in subjects with solid tumor malignancies with KRAS or NRAS mutations who are eligible for resection (Cohort A) or patients with metastatic cancers with KRAS or NRAS or BRAF mutations (Cohort B). Cohort C will involve patients with colorectal cancer having an extended RAS or BRAF mutation who are amenable for local-regional therapy of hepatic metastases with yttrium-90 (Y90) radioembolization to enhance the DNA damage.
The objective of the study is to investigate whether high-dose vitamin C infusion leads to pathological tumor response in resectable lung, colorectal, and pancreatic cancer (Cohort A) or objective tumor response in KRAS- or BRAF-mutant solid tumors (Cohort B). For Cohort C, the primary objective is to determine the maximal tolerated dose of the combination of high-dose vitamin C with Y90 radioembolization for patients with solid tumor malignancies and liver metastases amenable to local-regional therapy.
“We are optimistic. What we are expecting to see is some tumor shrinkage,” Cantley adds. “When this study is completed and we look at the data, we will learn more about how vitamin C works. If this approach shows good responses, then we can move on to larger trials.”
Those larger trials could be designed to determine optimal doses and to compare those results against standard of care or combination therapies, for example. “The patients enrolled in the study have disease that is very difficult to treat, and some are out of options,” Cantley says. “If we get tumor shrinkage and we increase the time it takes for the cancer to progress, that would be very exciting.”