Strong Like a Dinosaur

- Gastrointestinal symptoms and jaundice lead to pancreatic cancer diagnosis
- Second opinion at a large cancer center
- Chemotherapy with FOLFIRINOX
What I expected to be a wonderful 40th birthday filled with surprise and fun with my husband and two children ended up being a stressful, medical-related week of uncertainty and eventual diagnosis.
Starting in August 2019, I noticed an increase in bloating and gas. I went to my local urgent care, where the advanced practice registered nurse (APRN) checked me out but didn’t run any tests. He thought I was having irritable bowel syndrome and prescribed me a medication to take for a month. I took it, and although I didn’t notice any change in my bowels, my gas and bloating went away. I went back to my normal routine of working out heavily five to six days a week, running, lifting weights.
In November 2019, my bloating and gas came back, but not as severe. I had some upper back pain that would come and go, but I associated this with a herniated disc in my back, and possibly lifting incorrectly in the weight room. My stomach seemed off, and I couldn’t figure out if it was something that I was eating that was bothering me. I made an appointment with my doctor for November 25th. I noticed a darkening of my urine and my bowel movements were becoming lighter in color the weekend before. I called the doctor’s office on the 24th as I thought I was getting somewhat jaundiced; they told me that I was still okay to just come in the next day.
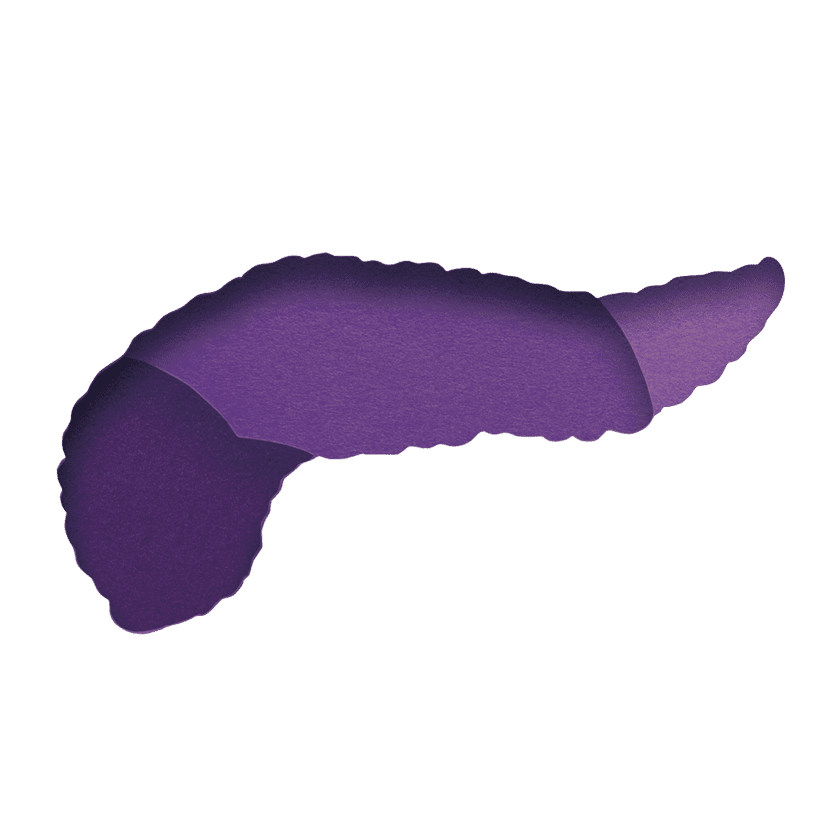
On Tuesday November 25th, 2019, I saw my primary doctor. She’s been my doctor for 10 years and she thought I might be slightly jaundiced, so she took some blood for lab work and ordered an ultrasound for the next morning. I thought it might possibly be my gall bladder since all of my female relatives on my mom’s side have had theirs removed. After my appointment, I went back to work. I ended up getting three different calls from my primary doctor after she got my lab results back. She talked with a surgeon and they wanted me to get an ultrasound that afternoon and then go immediately to see the surgeon. After some difficulties getting the ultrasound done because I hadn’t fasted, I went and saw the surgeon, where I heard “You have a spot on your pancreas.”
Confirming the Diagnosis
The next day I had another CT scan, an appointment with a surgeon, and an ERCP and biopsy. Then the wait. I saw the surgeon’s notes from the biopsy, which said a large spot that was noted. Without the official word, I knew what I faced. On my 40th birthday, December 3rd, 2019, I was diagnosed with pancreatic cancer. The first CT scan showed a tumor on the head of my pancreas. It was considered as locally advanced.
Although I live in Spokane, Washington, we went for a second opinion at Virginia Mason Medical Center in Seattle, a larger hospital where they see thousands of pancreatic cancer patients yearly. I met with oncologist Dr. Vincent Picozzi and surgeon Dr. Flavio Rocha (now at Oregon Health Science University). Both felt my cancer was more borderline resectable.
Starting Chemotherapy
Since the doctors at Virginia Mason offered the same chemotherapy as my local oncologist, we decided to continue treatment at home in Spokane, with an option to return to Virginia Mason if my treatment wasn’t working. Working with Dr. Corliss Newman at MultiCare in Spokane I began treatment with FOLFIRINOX, and I am just about to start my eighth round. After three rounds, my white blood cell count was a little too low and we added a growth factor called Zarxio. I am getting between three to five shots every 14 days. We are still trying to figure out the magic number to keep my numbers elevated. I wouldn’t say that the treatment has positively or negatively impacted my quality of life, but after four treatments it was positive news that the tumor had shrunk from 3.4cm x 4.2 cm to 2.8 cm x 3.3 cm. We send information to Dr. Rocha so he is aware of how I am doing. If my tumor shrinks enough we want Dr. Rocha to do the surgery because of his expertise. Dr. Newman and Dr. Rocha agreed I should have 12 sessions of chemo, and then surgery if possible.
The side effects that I have experienced have been primarily the neuropathy from the chemo, the sensation to fingers and not being able to drink cold liquids due to sensation in my throat. This usually lasts about 10 days after chemo, but if I reach into the freezer, my fingers will have the tingling temporarily. I have had some diarrhea associated with chemo, but much less than most. I will usually only have to take one to three Imodium total in-between treatments. There is some nausea the first three days after chemo, but the Zofran and Compazine manage this. Because I have a family history of abdominal cancers, I underwent genetic testing. One item showed up but it was listed as of “unknown significance.” My oncologist explained that at this point they don’t have enough information to determine if my pancreatic cancer is related to the family history of cancers.
A four-year-old neighbor was told that I was sick. Her response was that I will be okay because I am “strong like a dinosaur.” That has become our motto through this entire fight: #stronglikeadinosaur.
Andrea passed away from pancreatic cancer after sharing her story. She fought hard for her family. We offer our deepest sympathy.