Eating Right Can Help Your Pancreatic Cancer Fight

As the source of insulin that helps in the regulation of blood sugar and of enzymes that help break down fats, carbohydrates, and proteins, the pancreas is a key part of the digestive system.
So it’s not so surprising that cancer of the pancreas can bring with it significant nutritional challenges. Successfully addressing these challenges, however, brings multiple rewards: it can enable and enhance treatment, boost day-to-day well-being, and support healthy recovery.
A Dietitian’s Training and Experience Matters
When assembling a team to tackle your pancreatic cancer, a dietitian should be one of your first recruits, according to Maria Petzel, RD, CSO, LD, CNSC, a senior clinical dietitian at the MD Anderson Cancer Center. Ideally, he or she should have a CSO after their name, signifying they have received oncology nutrition certification, with more than 2,000 hours of clinical oncology experience under their belt. That experience comes in handy when assessing the needs of each patient, which differ from person to person, based on factors such as their body type, treatment history, surgical history, and amount of fat in their diet.
For pancreatic cancer patients it is important that the dietitian is well-educated in enzymes. Pancreatic enzymes help break down fats, proteins, and carbohydrates. A deficit of pancreatic enzymes can affect digestion, cause uncomfortable side effects, and weight loss. Symptoms of inadequate enzyme production include excessive gas, bloating, or indigestion after meals and changes in bowel movements such as light colored or yellow stools or stools that are frequent, floating, oily, or loose.
Fun Fact: A normally functioning pancreas secretes about eight cups of enzyme-containing pancreatic juice into the duodenum daily.
“Inadequate enzyme production can be fixed with pancreatic enzyme replacement therapy (supplementing with prescription enzymes), but it’s not a one-size-fits-all solution,” Petzel says. “Pancreatic cancer patients need to have someone on their healthcare team who can help individuals figure out what brand and dose works best to help minimize symptoms and get maximal digestion and absorption.”
Combating the Side Effects of Treatment
Weight loss due to pancreatic cancer is common, but its causes can be complicated. Some are related to the tumor itself, in which case surgery, chemotherapy, or radiation treatment can help. Others, however, are a result of such treatment.
Nausea, loss of appetite, or the change in taste that often accompany chemo or radiation therapy can be combated through diet and pharmaceutical strategies. These are most successful when tailored to each patient, Petzel explains. One person’s diarrhea could be caused by fat malabsorption due to pancreatic enzyme insufficiency, while another may be suffering the effects of lactose intolerance, bacterial overgrowth, chemotherapy, or dumping syndrome from surgical resection. Enzyme replacement may solve the problem for some patients, while a low-fat, low-fiber, and/or dairy-free diet might do the trick for others.
Maintaining a healthy weight for pancreatic cancer patients can be critical to the success of their treatment. “We know that patients who are able to maintain weight are more likely to get their scheduled doses of treatment,” Petzel adds.
Here is some general advice Petzel offers for patients:
- Consume small, frequent, balanced meals (not just snacks), six to eight per day, to help combat fatigue and weight loss. Schedule these meals for specific times. “Depending on your body to tell you it’s hungry is often not sufficient,” Petzel says.
- Avoid high-fat foods that are hard for your already taxed pancreas to handle.
- Watch your fiber. High intake of insoluble fiber food sources (whole grain breads/cereals, raw fruits with thick peels, raw vegetables, and nuts) can make foods move faster through and draw more water into the intestines, exacerbating diarrhea. Foods that contain soluble fiber, such as oat fiber, and high-pectin foods like applesauce and bananas, can help.
- Avoid sugary foods and portion out your carbs, mixing them with protein sources like low-fat dairy, beans, fish or seafood, poultry or lean red meat, to help with blood sugar stability.
- If your sense of taste has been altered due to treatment, experiment with different foods, textures, and flavors to determine what is most appealing.
- Keep hydrated by drinking clear beverages like water, juice, electrolyte replacement beverages, or broth. Beverages that contain calories, nutrients, and protein, such as smoothies or nutritional supplement drinks, can also be helpful for those who cannot stomach a meal.
- Stay active. “Even 5, 10, 15 minutes of physical activity, two or three times a day, can stimulate the appetite and promote the emptying of the stomach,” Petzel explains.
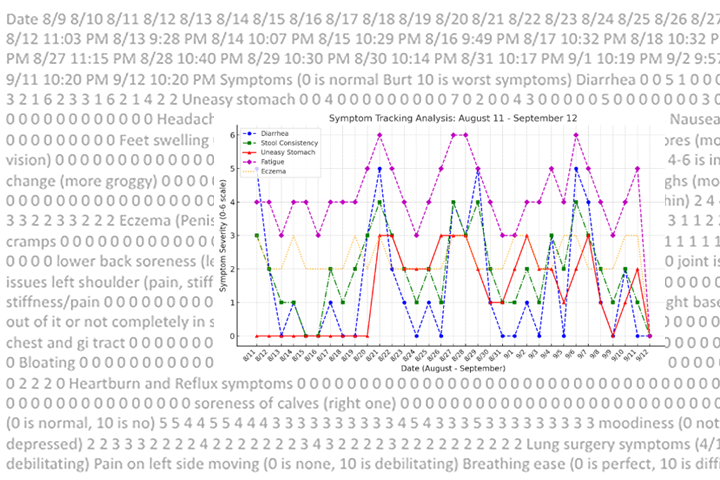
- Keep a daily diet journal recording foods eaten, weight, pancreatic enzymes used (and when, in relation to meals), frequency and consistency of bowel movements, and blood glucose readings, if applicable.
Additional nutritional advice can be found on the Academy of Nutrition and Dietetics Oncology Nutrition website. The American Institute for Cancer Research also provides some culinary inspiration in its recipe archives.
For other dietary suggestions, read the Disease Management article “How to Eat After a Whipple Procedure.”